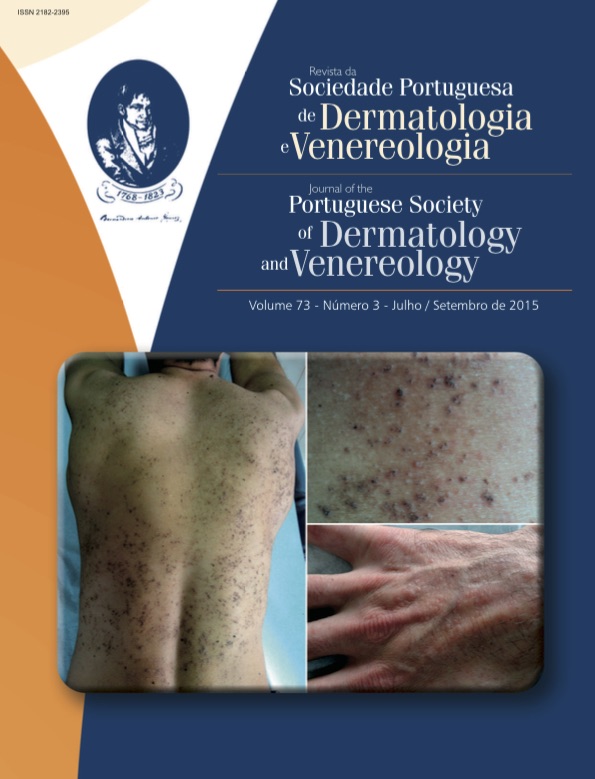
PITYRIASIS LICHENOIDES - REPORT OF TWO CASES SHOWING THE WIDE SPECTRUM OF PRESENTATION OF THIS RARE DISEASE
Abstract
Pityriasis lichenoides is a rare skin disease of unknown etiology, whose spectrum of clinical presentation varies from an acute form, pityriasis lichenoides et varioliformis acuta (PLEVA) to a more insidious and recurrent one, pityriasis lichenoides chronica (PLC). PLEVA, or Mucha-Habermann disease, has an acute onset of papules on the trunk, buttocks and proximal extremities that rapidly progress to vesicles or form hemorrhagic crusts, and may leave depressed scars. PLC, by contrast, has small scaly papules, asymptomatic or pruritic, which can develop over days, on the same distribution. The lesions may continue appearing and disappearing over months, sometimes causing post-inflammatory hypopigmentation. The patient does not usually evolve from a clinical form to another, tending to spontaneous healing or the cure comes after treatment. It is believed that pityriasis lichenoides is a hypersensitivity reaction to various infectious agents and with self-limiting clonal proliferation of T cells, wherein the immune response to the clone leads to clinical and pathological manifestations. It has been detected T-cell receptor gamma gene rearrangement (TCR-gamma) by PCR. Pathological exam shows typical changes of each presentation. This paper presents two very representative cases of this uncommon disease, showing the main features of each form of pityriasis lichenoides. Both had resolution with the use of Doxycycline.
Downloads
References
Fernandes NF, Rozdeba PJ, Schwartz RA, Kihiczak G, Lambert WC. Pityriasis lichenoides et varioliformis acuta: a disease spectrum. Int J Dermatol. 2010;49:257-61.
Kim JE, Yun WJ, Mun SK, Yoon GS, Huh J, Choi JH, et al. Pityriasis lichenoides et varioliformis acuta and pityriasis lichenoides chronica: comparison of lesional T-cell subsets and investigation of viral associations. J Cutan Pathol. 2011; 38:649-56.
Tomasini D, Tomasini CF, Cerri A, Sangalli G, Palmedo G, Hantschke M, et al. Pityriasis lichenoides: a cytotoxic T-cell-mediated skin disorder. Evidence of human parvovirus B19 DNA in nine cases. J Cutan Pathol. 2004; 31:531-8.
Kadin, ME. T-cell clonality in Pityriasis lichenoides. Arch Dermatol. 2002;138:1089-90.
Foss NT, Rocha LS, Roselino AM, Donadi EA. Pitiríase liquenóide – Estudos clínicos e imunogenéticos. FMUSP Ribeirão Preto. 2000 33:32-6.
Hood AF, Mark EJ. Histopathologic diagnosis of pityriasis lichenoides et varioliformis acuta and its clinical correlation. Arch Dermatol.1982; 118:478-82.
Rongioletti F, Delmonte S, Rebora A. Pityriasis lichenoides and acquired toxoplasmosis. Int J Dermatol. 1999; 38:367-76.
Truhan AP, Hebert AA, Esterly NB. Pityriasis lichenoides in children: therapeutic response to erythromycin. J Am Acad Dermatol 1986 15:66-70.
Piamphongsant T. Tetracycline for the treatment of pityriasis lichenoides. Br J Dermatol. 1974;91(3):319-22.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).