Desmoplastic Trichilemmoma arising on a Nevus Sebaceous of the Scalp
Abstract
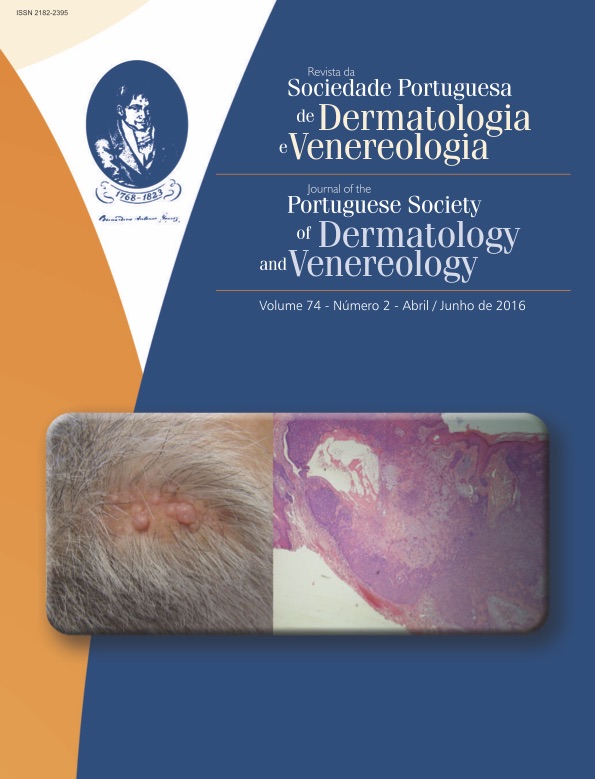
Originally described by Jadassohn in 1895, it was not until 1932 that the term “nevus sebaceous” was introduced by Robinson. It is a prevalent benign congenital hamartoma that classically evolves through discrete phases of growth and that, from the 4th to the 7th decade of life, can give rise in approximately 10 to 30% of cases to several epithelial neoplasms. Very seldom reported in this context, trichilemmomas are benign appendageal tumours that arise from or differentiate toward the outer root sheath epithelium of the normal hair follicle. Usually solitary, they present as verrucous, keratotic or smooth papules on the face, especially in the vicinity of the nose and lips. On clinical grounds, desmoplastic trichilemmomas, a rare benign histological sub-type of trichilemmomas, are easily taken for basal cell carcinomas, intradermal nevi, verrucae, cutaneous horns, sebaceous hyperplasia and squamous cell carcinomas; as far as pathology, differential diagnosis must include the desmoplastic variants of squamous and basal cell carcinomas, as well as trichilemmal carcinoma. A 56 year old Caucasian male presented with several asymptomatic pearly, translucid nodules and papules that had developed over the last 6 months within a congenital alopecic yellowish plaque of his scalp previously diagnosed, on clinical grounds, as a nevus sebaceous. Histopathological examination allowed to disclose a lobular neoplasm with the classic features of desmoplastic trichilemmoma. The case is iconographically depicted and the relevant literature is reviewed.
Downloads
References
Headington JT, French AJ. Primary neoplasms of the hair follicle: histogenesis and classification. Arch Dermatol. 1962;86:430-41.
Hunt SJ, Kilzer B, Santa Cruz DJ. Desmoplastic trichilemmoma: histologic variant resembling invasive carcinoma. J Cutan Pathol. 1990;17:45-52.
Rosõn E, Gomez Centeno P, Sanchez-Aguilar D. Desmoplastic trichilemmoma arising within a nevus sebaceous. Am J Dermatopathol.1998; 20: 495-7.
Mehregan AH, Pinkus H. Life history of organoid nevi. Arch Dermatol. 1965; 91:574-88.
Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceous: A study of 596 cases. J Am Acad Dermatol. 2000; 42:263-8.
TellecheaO, Reis JP, Poiares Baptista A. Desmoplastic trichilemmoma. Am J Dermatopathol. 1992; 14: 107-14.
Robinson SS. Nevus Sebaceous (Jadassohn): report of five cases. Arch Dermatol Syphilol.1932; 26:663-70.
Shapiro M, Johnson B Jr, Witmer W, Elenitsas R. Spiradenoma arising in a nevus sebaceous of Jadassohn: case report and literature review. Am J Dermatopathol.1999;21:462-7.
Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceous of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-7.
Groesser L, Herschberger E, Ruetten A, Ruivenkamp C, Lopriore E, Zutt M, et al. Postzygotic HRAS and KRAS mutations can cause nevus sebaceous and Schimmelpenning syndrome. Nat Genet. 2012; 44:783-7.
Aslam A, Salam A, Griffiths CE, McGrath JA. Nevus sebaceous: a mosaic RA Sopathy. Clin Exp Dermatol. 2014; 39:1-6.
Happle R. Nevus sebaceous is a mosaic RA Sopathy. J Invest Dermatol.2013; 133:597-600.
Jacqueti G, Requena L, Sanchez Yus E. Trichoblastoma is the most common neoplasm developed in nevus sebaceous of Jadassohn: a clinicopathologic study of a series of 155 cases. Am J Dermatopathol. 2000; 22:108-18.
Crowson AN, Magro CM. Basal cell carcinoma arising in association with desmoplastic trichilemmoma. Am J Dermatopathol. 1996; 18:43-8.
Afshar M, Lee RA, Jiang SI. Desmoplastic Trichelemmoma – A Report of Successful Treatment with Mohs Micrographic Surgery and a Review and Update of the Literature. Dermatol Surg. 2012; 38: 1867-71.
Illueca C, Monteagudo C, Revert A, Llombart-Bosch A. Diagnostic value of CD34 immunostaining in desmoplastic trichilemmoma. J Cutan Pathol. 1988; 25:435-9.
Fergin PE, Chu AC, MacDonald DM. Basal cell carcinoma complicating nevus sebaceous. Clin Exp Dermatol. 1981; 6:111-5.
Jones EW, Heyl T. Nevus sebaceous: a report of 140 cases with special regards to the development of secondary malignant tumors. Br J Dermatol. 1970; 82:99- 117.
Domingo J, Helwig EB. Malignant neoplasm associated with nevus sebaceous of Jadassohn. J Am Acad Dermatol. 1979; 1:545-56.
Xin H, Matt D, Qin JZ, Burg G, Böni R. The Sebaceous Nevus: A Nevus with Deletions of the PTCH Gene. Cancer Res.1999; 59: 1834-6.
Schweiger E, Spann CT, Weinberg JM, Ross B. A Case of Desmoplastic Trichilemmoma of the Lip Treated with Mohs Surgery. Dermatol Surg. 2004; 30:1062-4.
Sano DT, Yang JJ, Tebcherani AJ, Bazzo LA. A rare clinical presentation of Desmoplastic Trichilemmoma mimicking Invasive Carcinoma. An Bras Dermatol. 2014; 89:796-8.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).