Fatal Orbital Pyoderma Gangrenosum with Central Nervous System Involvement
Abstract
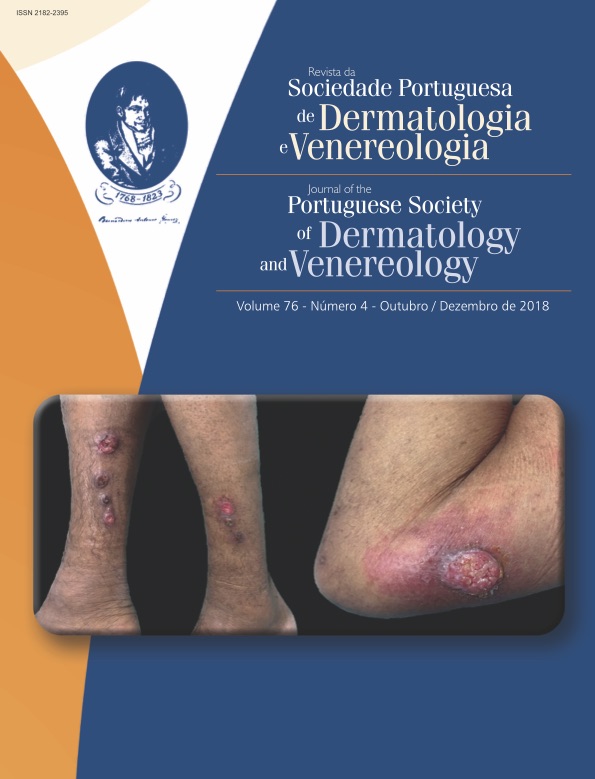
Pyoderma gangrenosum is a chronic inflammatory disease characterized by the development of a painful deep ulcer with undermined borders. Head and neck are rarely affected regions of the body and also usually associated with a worse prognosis. Corticosteroids are the mainstay of treatment although available options are not specific nor completely effective in pyoderma gangrenosum. We report the case of a 46-year-old patient with an aggressive orbital pyoderma gangrenosum with progressive extension to the central nervous system and insufficient response to treatment, ultimately leading to patient’s death.
Downloads
References
Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti
G. Pyoderma gangrenosum: an updated review.
J Eur Acad Dermatol Venereol. 2009; 23:1008-17. doi:10.1111/j.1468-3083.2009.03199.x.
Bryan CS. Fatal pyoderma gangrenosum with pathergy
after coronary artery bypass grafting. Tex Heart Inst J.
; 39:894-7.
Partridge ACR, Bai JW, Rosen CF, Walsh SR, Gulliver WP,
Fleming P. Effectiveness of systemic treatments for pyoderma
gangrenosum: a systematic review of observational
studies and clinical trials. Br J Dermatol. 2018;
:290-5. doi: 10.1111/bjd.16485.
Braswell SF, Kostopoulos TC, Ortega-Loayza AG. Pathophysiology
of pyoderma gangrenosum (PG): an updated
review. J Am Acad Dermatol. 2015; 73:691-8. doi:
1016/j.jaad.2015.06.021.
Mantovani L, Zauli S, Sarno O, Querzoli P, Corazza M,
Virgili A. Treatment of a relapsing facial pyoderma gangrenosum
(malignant pyoderma). Int J Dermatol. 2013;
:753-6. doi: 10.1111/j.1365-4632.2012.05755.x.
Leiphart PA, Lam CC, Foulke GT. Suppression of pathergy
in pyoderma gangrenosum with infliximab allowing
for successful tendon debridement. JAAD Case Rep.
; 4:98-100. doi: 10.1016/j.jdcr.2017.08.009.
Huang B, Melmed GY, Shih DQ. Facial ulceration in a
patient with Crohn's disease. Gastroenterology. 2012;
:1071, 1258. doi: 10.1053/j.gastro.2011.09.032.
Lana MA, Moreira PR, Neves LB. Wall-eyed bilateral
internuclear ophthalmoplegia (Webino syndrome) and
myelopathy in pyoderma gangrenosum. Arq Neuropsiquiatr.
;48:497-501.
Chanson P, Timsit J, Kujas M, Violante A, Guillausseau
PJ, Derome PJ, et al. Pituitary granuloma and pyoderma
gangrenosum. J Endocrinol Invest. 1990;13:677-81.
Ahn C, Negus D, Huang W. Pyoderma gangrenosum:
a review of pathogenesis and treatment. Expert
Rev Clin Immunol. 2018; 14:225-33. doi:
1080/1744666X.2018.1438269.
Ambooken B, Khader A, Muhammed K, Rajan U, Snigdha
O. Malignant pyoderma gangrenosum eroding the
parotid gland successfully treated with dexamethasone
pulse therapy. Int J Dermatol. 2014; 53:1536-8. doi:
1111/ijd.12519.
Sehgal R, Resnick JM, Al-Hilli A, Mehta N, Conway T,
Stratman EJ. Nasal septal and mucosal disease associated
with pyoderma gangrenosum in a cocaine
user. JAAD Case Rep. 2017; 3:284-7. doi: 10.1016/j.
jdcr.2017.05.004.
Maverakis E, Ma C, Shinkai K, Fiorentino D, Callen JP,
Wollina U, et al. Diagnostic Criteria of Ulcerative Pyoderma
Gangrenosum: A Delphi Consensus of International
Experts. JAMA Dermatol. 2018;154:461-6. doi:
1001/jamadermatol.2017.5980.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).