Cutaneous Manifestations of COVID-19: A Case Series from Brazil
Abstract
Introduction: Brazil has presented alarming and growing data on infection and deaths from SARS-CoV-2. There are more than 4 500 000 confirmed cases and more than 137 000 deaths ranking second in the world ranking of infected people. In addition to the involvement of the respiratory, cardiovascular, renal and neurological systems, this virus also causes non-specific skin lesions in same patients. Little is known about the pathophysiology of cutaneous involvement. At this moment, we cannot predict a difference in prognosis based on skin lesions.
Methods: We conducted an observational case study of 25 patients affected by SARS-CoV-2 who had dermatological lesions. We described the clinical and epidemiological characteristics of each case, demonstrating the polymorphism of the skin lesions and also making a correlation with the chronology of presented systemic symptoms.
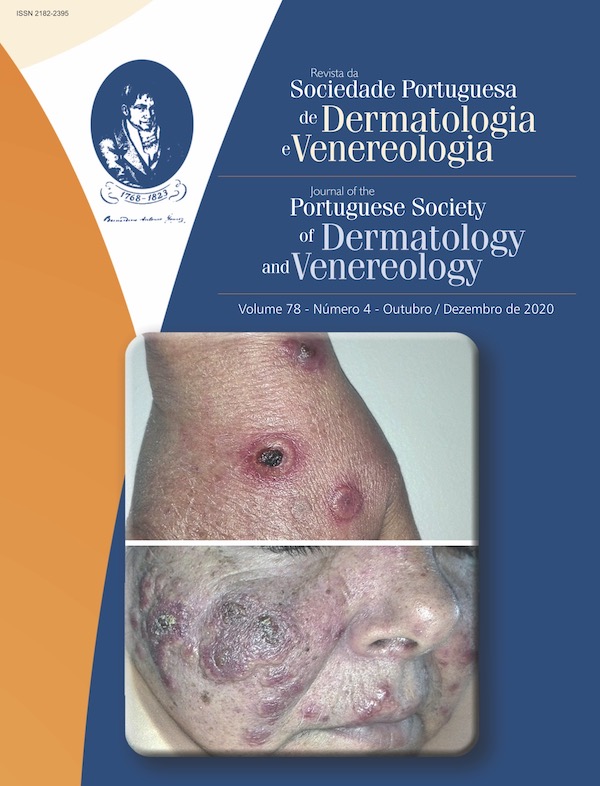
Results: Twenty five cases of COVID-19 with cutaneous manifestations (urticaria, erythematous rash, maculopapular eruption, pruritus, erythema multiforme-like lesions, dyshidrotic eczema) were observed during, after and before systemic symptoms. A few cases with skin involvement were also observed as isolated symptoms of the viral infection. These data demonstrate the clinical polymorphism related to skin involvement of patients infected with SARS-CoV-2, emphasizing the importance of clinical suspicion by dermatologists when handling suspected cases in the current epidemiological scenario.
Conclusion: Although the number of cases in the world stage seems to be regressing, infection by SARS-CoV-2 will be part of the dermatologist's daily routine. As long as we do not have a widely available vaccine and the pandemic takes on an endemic profile, we need to be aware of these manifestations, not only for the proper diagnosis, indication of patient isolation, as well as all the necessary biosafety procedures in dermatology clinics.
Downloads
References
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. doi: 10.1016/S0140-6736(20)30183-5. Erratum in: Lancet. 2020;395:496. doi: 10.1016/S0140-6736(20)30252-
-X.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-5. doi:10.1016/j.ijid.2020.03.017.
Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging. 2020;12:6049-57. doi:10.18632/aging.103000
Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9:45. doi:10.1186/s40249-020-00662-x.
Kolivras A, Dehavay F, Delplace D, Feoli F, Meiers I, Milone L, et al., Coronavirus (COVID-19) infection induced chilblains: a case report with histopathological findings, JAAD Case Rep.2020;6:489-92. doi: 10.1016/j.jdcr.2020.04.011.
Wambier CG, Goren A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is likely to be androgen mediated. J Am Acad Dermatol. 2020;83:308-9. doi: 10.1016/j.jaad.2020.04.032.
BBC News Brasil. Coronavírus: o mapa que mostra o alcance mundial da doença. Coronavirus Brasil. [accessed 07 October 2020] Available from: https://www.bbc.com/portuguese/internacional-51718755
Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212-3. doi:10.1111/jdv.16387.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-20. doi:10.1056/NEJMoa2002032.
[accessed 07 October 2020] Available from: https://covid.saude.gov.br.
Bouaziz JD, Duong T, Jachiet M, Velter C, Lestang P, Cassius C, et al. Vascular skin symptoms in COVID-19: a french observational study. J Eur Acad Dermatol Venereol. 2020 (in press). doi: 10.1111/jdv.16544.
Galván Casas C, Català A, Carretero Hernández G, Carretero Hernández G, Rodríguez-Jiménez P, Fernández-Nieto D, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183:71-7. doi: 10.1111/bjd.19163. Epub 2020 Jun 10.
Copyright (c) 2020 Journal of the Portuguese Society of Dermatology and Venereology

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).