ANOGENITAL WARTS IN CHILDREN – A CHALLENGING DIAGNOSIS
Abstract
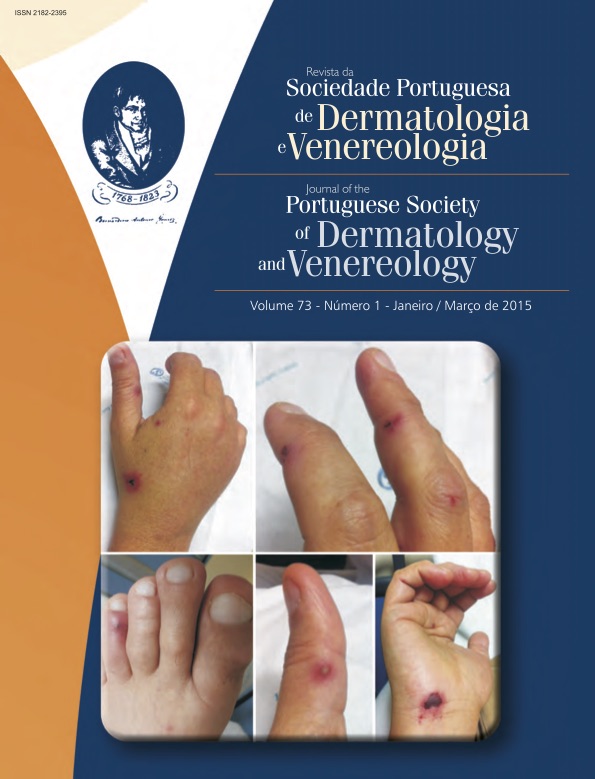
Anogenital warts (AGW) are benign tumors of the skin and mucosal epithelium caused by human papilloma virus infection. There is a growing prevalence of anogenital warts in the pediatric population, resulting from vertical transmission, auto or heteroinoculation. The diagnosis is primarily clinical and biopsy is reserved for doubtful diagnosis. Most lesions resolve spontaneously over time but recurrence is frequent, even after treatment, so watchful waiting is a valid option. The possibility of sexual abuse in children with anogenital warts represents a challenge in clinical practice. Most authors consider that the diagnosis of sexual abuse relies mainly on a complete anamnesis, a skilled interviewer and a thorough physical examination. There is general consensus that the probability of abuse increases with the child’s age, especially over 5 years of age. For children under 2 years, nonsexual human papilloma virus transmission should be strongly considered, in the absence of traumatic signs, other sexually transmitted diseases or a consistent history of abuse. However, sexual abuse cannot be ruled out at any age, so a careful follow-up is required, considering all the previously mentioned factors.
Downloads
References
Sexually Transmitted Diseases Treatment Guidelines. MMWR. 2010;59:69-74.
Marcoux D, Nadeau K, McCuaig C, Powell J, Oligny LL. Pediatric anogenital aarts: a 7-year review of children referred to a tertiary care hospital in Montreal, Canada. Pediatr Dermatol. 2006; 23(3):199-207.
Sinclair KA, Woods CR, Sinal SH. Venereal warts in children. Pediatr Rev. 2011; 32:115-21.
Monk BJ, Tewari KS. The spectrum and clinical sequelae of human papillomavirus infection. Gynecol Oncol. 2007; 107(Supl1):S6-S13.
Syrjanen S. Current concepts on human papillomavirus infections in children. APMIS. 2010; 118(6-7):494-509.
Syrjanen S, Puranen M. Human papillomavirus infections in children: the potential role of maternal transmission. Crit Rev Oral Biol Med. 2000; 11(2):259-74.
Burns T, Breathnach S, Cox N, Griffiths C. Rook’s Textbook of Dermatology. 7th ed. Oxford: Blackwell Publishing; 2004.
Jones V, Smith SJ, Omar HA. Nonsexual transmission of anogenital warts in children: a retrospective analysis. Scientific World J. 2007; 7:1896-9.
Rombaldi RL, Serafini EP, Mandelli J, Zimmermann E, Losquiavo KP. Perinatal transmission of human papilomavirus DNA. Virol J. 2009; 6:83.
Obalek S, Jablonska S, Favre M, Walczak L, Orth G. Condylomata acuminata in children: frequent association with human papillomaviruses responsible for cutaneous warts. J Am Acad Dermatol. 1990; 23:205-13.
Obalek S, Jablonska S, Orth G. Anogenital warts in children. Clin Dermatol. 1997; 15:369-76.
Jayasinghe Y, Garland SM. Genital warts in children: what do they mean? Arch Dis Child. 2006; 91:696-700.
Bodemer C. Human papillomavirus infection. In: Harper J, Orange A, Prose N, editors. Textbook of pediatric dermatology. Oxford: Blackwell Science; 2000. p. 1087-9.
Smith EM, Parker MA, Rubenstein LM, Haugen TH, Hamsikova E, Turek LP. Evidence for vertical transmission of HPV from mothers to infants. Infect Dis Obstet Gynecol. 2010; 326369.
Jesus LE, Cirne Neto OL, Monteiro do Nascimento LM, Costa Araújo R, Agostinho Baptista A. Anogenital warts in children: sexual abuse or unintentional contamination? Cad. Saúde Pública. 2001; 17(6):138391.
Smith EM, Johnson SR, Cripe T, Perlman S, McGuinness G, Jiang D, et al. Perinatal transmission and maternal risks of human papillomavirus infection. Cancer Detect Prevent. 1995; 19(2):196-205.
Benjamin L, Levy M, Ofori A. Condylomata acuminata (anogenital warts in children). In: Basow, DS, editor. UpToDate. Waltham: UpToDate;2014. [consultado em Junho 2014]. Disponível em http://www.uptodate.com
Sterling JC, Handfield-Jones S, Hudson PM. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001; 144:4-11.
Kellogg N. The evaluation of sexual abuse in children. Pediatrics. 2005; 116:506-12.
Fortin K, Jenny C. Sexual Abuse. Pediatr Rev. 2012; 33:19-32.
Sinclair KA, Woods CR, Kirse DJ, Sinal SH. Anogenital and respiratory tract human papillomavirus infections among children: age, gender, and potential transmission through sexual abuse. Pediatrics. 2005; 116(4):815-25.
Drezett J, Vasconcellos R, Pedroso D, Blake M, Oliveira A, Abreu L: Transmission of anogenital warts in children and association with sexual abuse. J Hum Growth Dev. 2012; 22(1):34-40.
Girardet RG, Lahoti S, Howard LA, Fajman NN, Sawyer MK, Driebe EM, et al. The epidemiology of sexually transmitted infections in suspected child victims of sexual assault. Pediatrics. 2009; 124(1):79-86.
Handley J, Hanks E, Armstrong K, Bingham A, Dinsmore W, Swann A, et al. Common association of HPV 2 with anogenital warts in prepubertal children. Pediatr Dermatol. 1997; 14:339-43.
Lacey CJN, Woodhall SC, Wikstrom A, Ross J. 2012 European guideline for the management of anogenital warts. JEADV. 2013; 27:e263-e270.
Fiorillo L. Therapy of pediatric genital diseases. Dermatol Ther. 2004;17(1):117-28.
Culton DA, Morrell DS, Burkhart CN. The management of condyloma acuminata in the pediatric population. Pediatr Ann. 2009; 38:368-72.
Ko J, Bigby M. Randomized controlled trial of cryotherapy with liquid nitrogen vs topical salicylic acid vs wait-and-see for cutaneous warts. Arch Dermatol. 2012; 148(7):840-2.
Le Cleach L, Trinquart L, Penso-Assathiany D, Chosidow O. Comparative effectiveness of cryotherapy and salicylic acid for plantar warts. Arch Dermatol. 2012; 148(11):1311-3.
Brandt H, Patriota R, Junior W, Fernandes J, Criado P. Tratamento do papiloma vírus humano na infância com creme de imiquimode a 5%. An Bras Dermatol. 2009; 84(5):549-53.
Moresi JM, Herbert CR, Cohen BA. Treatment of anogenital warts in children with topical 0.05% podofilox gel and 5% imiquimod cream. Pediatr Dermatol. 2001; 18:448-52.
Infarmed. Imiquimod – Resumo das Características do Medicamento (aprovado em 27/9/2012). [consultado 1 de Março 2014] Disponível em:http://www.infarmed.pt/infomed
Direção-Geral da Saúde. Programa Nacional de Vacinação 2012 – Norma nº 040/2011 de 21/12/2011. [consultado 23 abril 2014] [Disponível online em www.dgs.pt, acedido em 23 Abril 2014].
Howell-Jones R, Soldan, K, Wetten S, Mesher D, Williams T, Gill ON, et al. Declining genital warts in young women in England associated with HPV 16/18 vaccination: an ecological study. J Infect Diseases. 2013; 208:1397-403.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).