CHILDHOOD NON-LANGERHANS CELL HISTIOCYTOSIS - AN ATYPICAL CASE
Abstract
Introduction: Histiocytoses correspond to a heterogeneous group of disorders characterized by the proliferation and infiltration of histiocytes in tissues. For years, many of the histiocytoses where known by numerous names, reflecting the lack of understanding regarding their origin.
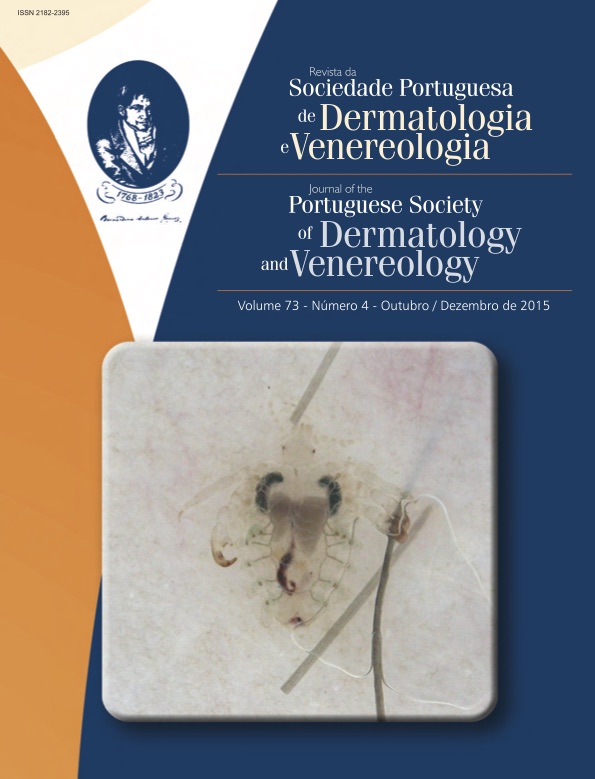
Case report: A previously healthy, 4-month-old infant presented a cutaneous lesion of progressive growth on his nose since 1 month ago. The mother has a diagnosis of Sjögren syndrome. On examination, there was a firm well- -defined erythematous plaque with 30 mm of diameter and raised edges, on the bridge of the nose. At the left cheek, left thoracic region and right arm there were also small erythematous papules with 5 days of evolution. The analytical study showed elevated antinuclear antibodies and anti-SS-A. Histopathological examination confirmed the diagnosis of non-Langerhans cells histiocytosis. Progressively, more annular erythematous papules and plaques appeared scattered over the face, trunk and limbs with spontaneous resolution of the first lesion on the nose. About 2 months after the initial evaluation, all lesions had regressed spontaneously, with normalization of analytical study at one year-old.
Conclusion: Many authors believe that the different subtypes of histiocytosis represent only different stages of the same disease. Immunophenotyping of histiocytosis does not always identify the subtype involved, making the occurrence of atypical cases frequent.
Downloads
References
Goodman WT, Barret TL. Disorders of Langerhans cells and Macrophages. Chapter 91: p. 1529-46.
Gianotti F, Caputo R. Histiocytic syndromes: a review. J Am Acad Dermatol. 1985; 13: 383-404.
Newman B, Weimin H, Nigro K, Gilliam AC. Aggressive histiocytic disorders that can involve the skin. J Am Acad Dermatol. 2007; 56:302-16.
Marrogi AJ, Dehner LP, Coffin CM. Benign cutaneous histiocytic tumors in childhood and adolescence, excluding Langerhans’s cells proliferations. Am J Dermatopathol. 1990; 12:221-33.
Sidoroff A, Zelger B, Steinher H. Indeterminate cell histiocytosis. Br J Dermatol. 1996; 134:525-32.
Jih DM, Salcedo SL, Jaworsky C. Benign cephalic histiocytosis: a case report and review. J Am Acad Dermatol. 2002; 47:908-13.
Gianotti F, Alessi E, Caputo R. Benign cephalic histiocytosis. Arch Dermatol. 1986; 122:1038-43.
Winkelmann RK, Muller SA. Generalized eruptive histiocytoma: a benign popular histiocytic reticulosis. Arch Dermatol. 1963; 88:586-96.
Helwig EB, Hackney VC. Juvenile xanthogranuloma. Am J Pathol. 1954; 30:625-6.
Wood AJ, Wagner VU, Abbott JJ, Gibson LE. Necrobiotic xanthogranuloma. A review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol. 2009; 145:279-84.
Gorman JD, Danning C, Schumacher HR, Klippel JH, Davis JC Jr. Multicentric reticulohistiocytosis: case report with immunohistochemical analysis and literature review. Arthritis Rheum. 2000; 43:930-8.
Caputo R, Veraldi S, Grimalt R, Gianotti R, Tosti A, Varotti C, et al. The various clinical patterns of xanthoma disseminate. Considerations on seven cases and review of the literature. Dermatology. 1995; 190:19-24.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).