Multinucleate Cell Angiohistiocytoma
Abstract
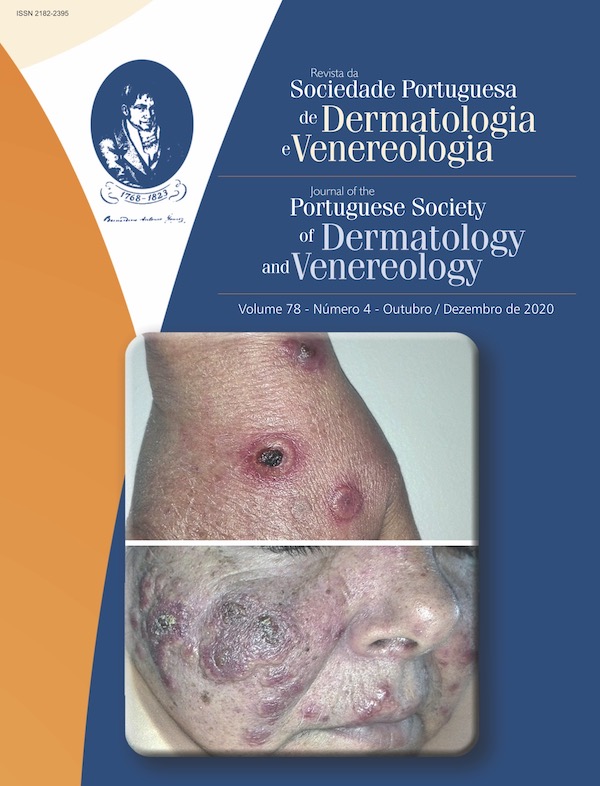
Multinucleated cell angiohistiocytoma (MCAH) is a rare clinical entity whose pathogenesis is not fully understood. It is more common in middle-aged women and is characterized by erythematoviolaceous papules or nodules, usually asymptomatic and predominantly located in the extremities. Histopathology is essential for making the diagnosis, consisting of typical alterations in the dermis, namely the proliferation of small vessels and the presence of multinucleated giant cells. Evolution is benign, although persistent, with few reported cases of spontaneous remission. We present the case of a 48-year-old man with MCAH, who exhibited asymptomatic papules and nodules grouped on the back of both hands, with a year of evolution. The diagnosis was made after histopathology, which excluded other differential diagnoses. With this case report, we intend to contribute to the knowledge about this entity and highlight the interconnection of clinical observation and histopathologic analysis.
Downloads
References
Smith NP, Jones EW. Multinucleate cell angiohistiocytoma - a new entity. Br J Dermatol. 1985; 113:15-15. doi:10.1111/j.1365-2133.1985.tb12966.x
Frew JW. Multinucleate cell angiohistiocytoma: clinicopathological correlation of 142 cases with insights into etiology and pathogenesis. Am J Dermatopathol. 2015; 37:222-8. doi:10.1097/DAD.0000000000000075
Wang M, Abdul-Fattah B, Wang C, Zhao Y, Qu X, Al-Muriesh M, et al. Generalized multinucleate cell angiohistiocytoma: case report and literature review. J Cutan Pathol. 2017; 44:125-34. doi:10.1111/cup.12853
Pérez LP, Zulaica A, Rodríguez L, Campo MC, Peñaranda JM, Fernández-Redondo V, et al. Multinucleate cell angiohistiocytoma.
Report of five cases. J Cutan Pathol. 2006; 33:349-52. doi:10.1111/j.0303-6987.2006.00428.x
Grgurich E, Quinn K, Oram C, McClain R, Lountzis N. Multinucleate cell angiohistiocytoma: Case report and literature review. J Cutan Pathol. 2019; 46:59-61. doi:10.1111/cup.13361
Cribier B, Gambini C, Rainero M, Grosshans E. Multinucleate cell angiohistiocytoma. A review and report of four cases. Acta Derm Venereol. 1995; 75:337-9. doi:10.2340/0001555575337339
Teixeira V, Serra D, Pereira N, Tellechea O. Multinucleate cell angiohistiocytoma: a new case report with dermoscopy. Dermatol Online J. 2014; 20:3.
Rato M, Monteiro AF, Parente J, Aranha J. Case for diagnosis. Multinucleated cell angiohistiocytoma. An Bras Dermatol. 2018; 93:291-3. doi:10.1590/abd1806-4841.20186821
Cesinaro AM, Roncati L, Maiorana A. Estrogen receptor alpha overexpression in multinucleate cell angiohistiocytoma: new insights into the pathogenesis of a reactive process. Am J Dermatopathol. 2010; 32:655-9. doi: 10.1097/DAD.0b013e3181d3ca49
Roy SF, Dong D, Myung P, McNiff JM. Multinucleate cell angiohistiocytoma: A clinicopathologic study of 62 cases and proposed diagnostic criteria. J Cutan Pathol. 2019; 46:563-9. doi:10.1111/cup.13463
Valerón-Almazán P, Dehesa L, Santana N, Vilar J, Carretero G. Hallazgos dermatoscópicos del angiohistiocitoma de células multinucleadas: ¿una variante de dermatofibroma? Actas Dermo-Sifiliográficas. 2011; 102:69-71. doi:10.1016/j.ad.2010.04.013
Thornsberry LA, English JC. Etiology, Diagnosis, and Therapeutic Management of Granuloma Annulare: An Update. Am J Clin Dermatol. 2013; 14:279-90. doi:10.1007/s40257-013-0029-5
Gibson LE, el-Azhary RA. Erythema elevatum diutinum. Clin Dermatol. 2000; 18:295-9.doi: 10.1016/S0738-081X(99)00120-0
Sass U, Noel JC, André J, Simonart T. Multinucleate cell angiohistiocytoma: report of two cases with no evidence of human herpesvirus-8 infection. J Cutan Pathol. 2000; 27:258-61. doi:10.1034/j.1600-0560.2000.027005258.x
Shields JA, Eagle RC, Shields CL, Sohmer KK. Multinucleate Cell Angiohistiocytoma of the Orbit. Am J Ophthalmol. 1995; 120: 402-3. doi:10.1016/S0002-9394(14)72178-6
Rawal YB, Anderson KM, Rawal SY. Multinucleate cell angiohistiocytoma: an uncommon mucosal tumour. Clin Exp Dermatol. 2009; 34:333-6. doi:10.1111/j.1365-2230.2008.02939.x
Copyright (c) 2020 Journal of the Portuguese Society of Dermatology and Venereology

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).