UREMIC CALCIPHYLAXIS UNDER THE CALCIMIMETIC CINACALCET
Abstract
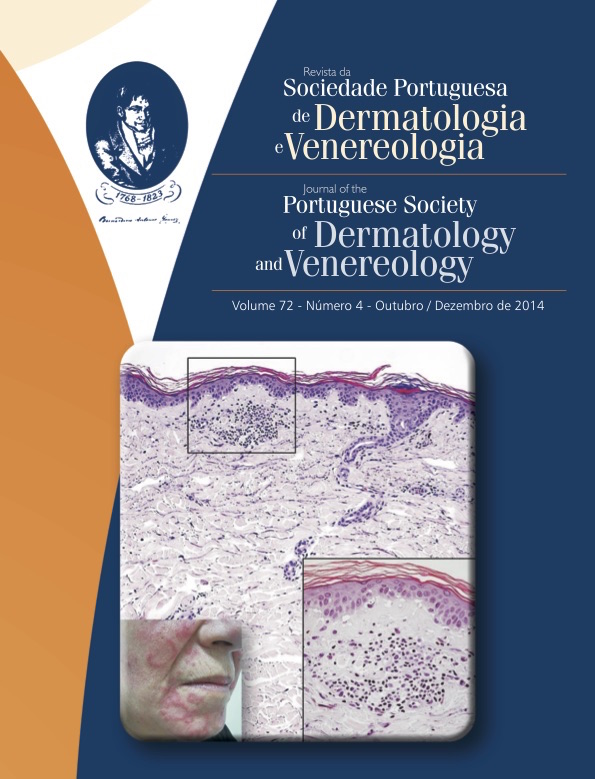
Uremic calciphylaxis is a rare but serious complication of dialysis patients. Its pathogenesis is not completely understood, although many risk factors have been identified, such as hyperparathyroidism. Cinacalcet (a calcimimetic agent) is used to keep calcium, phosphorus and PTH within the normal range. A 72-year old female patient, under hemodialysis for 15 years with hyperphosphatemia, normocalcemia and hyperparathyroidism despite therapy with cinacalcet and sevelamer, presented with several painful ulcerated lesions of the right leg, with a geographical configuration, central necrotic surface and hemorrhagic borders that progressed for 6 weeks. Cutaneous biopsy revealed vascular deposits of calcium in deep dermal and hypodermal vessels, confirming the clinical diagnosis of calciphylaxis. The necrotic borders of the ulcer improved when cinacalcet and sevelamer were administered in maximum doses. However, the patient passed away in consequence of comorbidities. We report a case in which cinacalcet was ineffective in controlling the phosphate and calcium abnormalities in an hemodialysis patient and, consequently, his cutaneous lesions.
Downloads
References
Fairley JA. Calcifying and ossifying disorders of the skin. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology 2nd ed. Philadelphia: Mosby Elsevier;2008.p. 653-9.
Pallure V, Comte C, Leray-Mouragues H, Dereure O. Cinacalcet as first-line treatment for calciphylaxis. Acta DermVenereol. 2008; 88:62-3.
Nunley J, Khjan S, Vinson R, Meffert J , Gelfand J, Elston D Calcyphylaxis. Medscape. 2013. [consultado em 16 Julho 2014]. Disponível em http://emedicine.medscape.com/article/1095481-overview.
Mohammed I, Sekar V, Bubtana A, Mitra S, Hutchison A. Proximal calciphylaxis treated with calcimimetic “cinacalcet”. Nephrol Dial Transplant. 2008;(23):387-9.
Velasco N, MacGregor M, Innes A, MacKay I. Successful treatment of calciphylaxis with cinacalcet – an alternative to parathyroidectomy? Nephrol Dial Transplant. 2006; 21:1994-2004.
Robinson M, Augustine J, Korman N. Cinacalcet for the treatment of calciphylaxis. Arch Dermatol. 2007; 143(2):152-4.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).