Gemcitabine-Induced Bullous Acral Erythema
Abstract
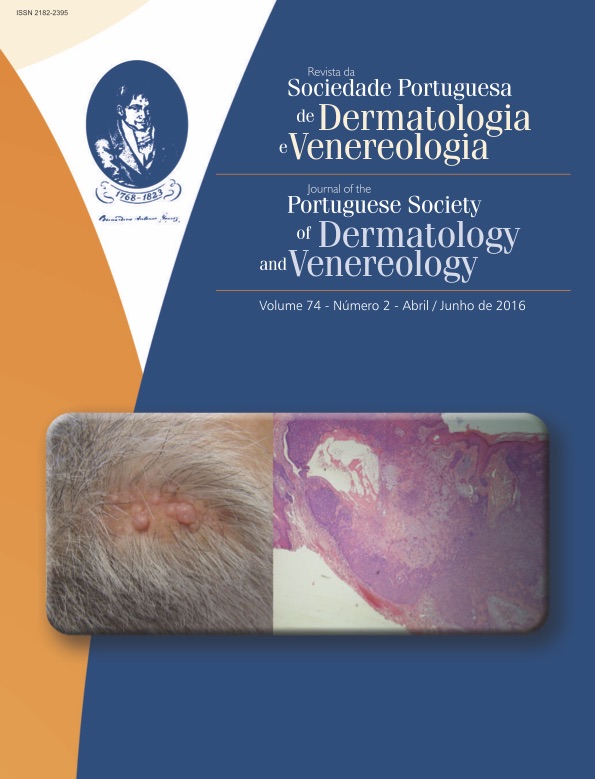
Chemotherapy-induced acral erythema is characterized by areas of painful erythema affecting predominantly hands and feet, and in severe cases bullous lesions may develop. Gemcitabine is frequently responsible for cutaneous side effects, but these are usually mild and transient. We report a patient under palliative chemotherapy for pancreatic ductal adenocarcinoma with gemcitabine, who presented large bullous lesions on both feet, but of larger size on the left. Histopathology was consistent with acral erythema. The bullous variant of chemotherapy-induced acral eythema is a rare reaction, and although described for structurally similar cytotoxic agents, it has not been reported in association with gemcitabine. In our case, the patient’s medical history of significant peripheral arterial disease may have also played an important role in the overall clinical presentation.
Downloads
References
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981; 30:239-45.
Rodriguez Martin AM, Guirao Arrabal E, Jimenez Puya R, Velez Garcia-Nieto A. Paraneoplastic Acral Vascular Syndrome. Actas Dermosifiliogr. 2015; 106:601-2.
Lotem M, Hubert A, Lyass O, Goldenhersh MA, Ingber A, Peretz T, et al. Skin toxic effects of polyethylene glycol-coated liposomal oxorubicin. Arch Dermatol. 2000;136:1475-80.
Bolognia JL, Cooper DL, Glusac EJ. Toxic erythema of chemotherapy: a useful clinical term. J Am Acad Dermatol. 2008; 59:524-9.
Marques Pinto G. Medicamentos que induzem ou agravam doenças cutâneas crónicas. Trab Soc Port Dermat Venereol. 2010; 68:11-44.
Revenga Arranz F, Fernandez-Duran DA, Grande C, Rodriguez Peralto JL, Vanaclocha Sebastian F. Acute and painful erythema of the hands and feet. Acral erythema induced by chemotherapy. Arch Dermatol. 1997; 133:499-500, 2-3.
Azurdia RM, Clark RE, Friedmann PS. Chemotherapy-induced acral erythema (CIAE) with bullous reaction. Cain Exp Dermatol. 1999;24:64-6.
Waltzer JF, Flowers FP. Bullous variant of chemotherapy-induced acral erythema. Arch Dermatol. 1993; 129:43-5.
Balagula Y, Lacouture ME, Cotliar JA. Dermatologic toxicities of targeted anticancer therapies. J Support Oncol. 2010; 8:149-61.
Robert C, Sibaud V, Mateus C, Cherpelis BS. Advances in the management of cutaneous toxicities of targeted therapies. Semin Oncol. 2012; 39:227-40.
Aapro MS, Martin C, Hatty S. Gemcitabine--a safety review. Anticancer Drugs. 1998; 9:191-201.
Chu CY, Yang CH, Chiu HC. Fixed erythrodysaesthesia plaque due to gemcitabine and epirubicin treatment. Acta Derm Venereol. 2002; 82:147-8.
Li J, Ko CJ, Saif MW. Recurrent cutaneous toxic erythema induced by gemcitabine in a patient with pancreatic cancer. Cutan Ocul Toxicol. 2009; 28:144-8.
Imen A, Amal K, Ines Z, Sameh el F, Fethi el M, Habib G. Bullous dermatosis associated with gemcitabine therapy for non-small-cell lung carcinoma. Respir Med. 2006;
:1463-5.
Jidar K, Ingen-Housz-Oro S, Beylot-Barry M, Paul C, Chaoui D, Sigal-Grinberg M, et al. Gemcitabine treatment in cutaneous T-cell lymphoma: a multicentre study of 23 cases. Br J Dermatol. 2009; 161:660-3.
Janusch M, Fischer M, Marsch W, Holzhausen HJ, Kegel T, Helmbold P. The hand-foot syndrome--a frequent secondary manifestation in antineoplastic chemotherapy. Eur J
Dermatol. 2006; 16:494-9.
Brandes A, Reichmann U, Plasswilm L, Bamberg M. Timeand dose-limiting erysipeloid rash confined to areas of lymphedema following treatment with gemcitabine--a report
of three cases. Anticancer Drugs. 2000; 11:15-7.
Voorburg AM, van Beek FT, Slee PH, Seldenrijk CA, Schramel FM. Vasculitis due to gemcitabine. Lung Cancer. 2002; 36:203-5.
Venat-Bouvet L, Ly K, Szelag JC, Martin J, Labourey JL, Genet D, et al. Thrombotic microangiopathy and digital necrosis: two unrecognized toxicities of gemcitabine. Anticancer Drugs. 2003; 14:829-32.
Dasanu CA. Gemcitabine: vascular toxicity and prothrombotic potential. Expert Opin Drug Saf. 2008; 7:703-16.
Scheithauer W, Blum J. Coming to grips with hand-foot syndrome. Insights from clinical trials evaluating capecitabine. Oncology. 2004; 18:1161-8, 73; discussion 73-6,81-4.
Kanai M, Matsumoto S, Nishimura T, Matsumura Y, Hatano E, Mori A, et al. Premedication with 20 mg dexamethasone effectively prevents relapse of extensive skin rash associated with gemcitabine monotherapy. Ann Oncol. 2010; 21:189-90.
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).