The Importance of Dedicated Dermatology Clinics in the Care of Organ Transplant Recipients.
Abstract
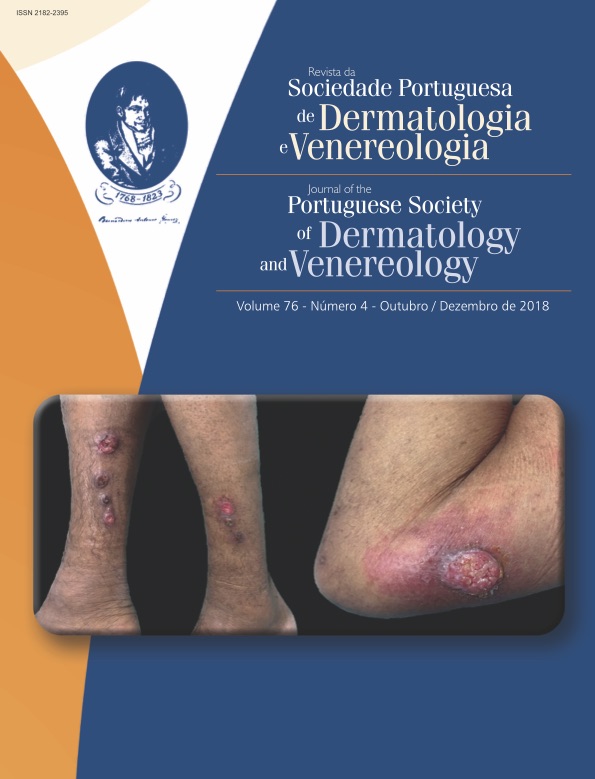
Organ transplant recipients have a high risk of skin cancer associated with immunosuppressive therapy and ultraviolet radiation. The incidence of non-melanoma skin cancer, in particular is up to 65-times higher than for the normal population. Field cancerization of sun- exposed skin is also a major health issue in these patients1.
In Portugal there were 895 solid organ transplants in 2017, with the majority being kidney (529) and liver (259)2.
There are already several publications concerning skin cancer in Portuguese organ transplant recipients, reporting a prevalence of non-melanoma skin cancer ranging from 15% to 25% in renal transplant recipients3,4,5and 8% in one series6that included more liver transplant recipients with relatively less immunosuppression.
The sunny geographical location and sun exposure habits, namely the poor knowledge and adherence to photoprotective measures, such as hats, long-sleeved clothes or sunscreen while on outdoor work or leisure activities, pose serious difficulties for skin cancer prevention in this population. In one study concerning knowledge of sun protective measures in a population of Portuguese transplant recipients7, 29% did not know that their risk of skin cancer was increased, and 25% of those who went to the beach stayed there between 11.30 and 16:00 pm. Not surprisingly, only 8% consulted a dermatologist in the first year after transplant7.
Different organizations like the Skin Care in Organ Transplant Recipients - Europe (SCOPE) or the International Transplant Skin Cancer Collaborative (ITSCC) together with institutions such as the British National Institute for Health and Clinical Excellence (NICE)8,9,10, recommend initial assessment of these patients by a dermatologist and providing them with education on photoprotection and self-examination of the skin. These patients also need regular follow-up with time intervals defined by their previous history of skin cancer and the presence of field cancerization of their sun-exposed skin. In such patients with previous skin cancer and detectable field cancerization, some authors11propose three months as time interval between appointments.
Dedicated or specialist dermatology clinics for organ transplantation are recommended11,12,and have also been shown to improve compliance with photoprotection13. Their introduction in the main Portuguese referral hospitals for transplantation would allow earlier dermatological care, inclusion of dermatology among the specialties that collaborate in the transplant teams and reduction of the burden of skin cancer in these patients, saving lives and costs.
Downloads
References
Zwald FO, Brown M. Skin cancer in solid organ transplant
recipients: advances in therapy and management:
part I. Epidemiology of skin cancer in solid organ transplant
recipients. J Am Acad Dermatol. 2011; 65: 253-
doi: 10.1016/j.jaad.2010.11.062.
Doação e Transplantação de Órgãos. Atividade Nacional
– 2017. [Acedido em maio de 2018].
Disponível em: http://www.ipst.pt/files/TRANSPLANTACAO/
DOACAOETRANSPLANTACAO/Colheita_e_
Transplantacao_2017_22janeiro.pdf.
Garrido PM, Borges-Costa J. Skin disorders in renal
transplant recipients: a retrospective study. An Bras
Dermatol. 2017; 92: 638-41. doi: 10.1590/abd1806-
20176040.
Borges-Costa J, Vasconcelos JP, Travassos AR, Guerra
J, Santana A, Weigert A, et al. Skin cancer in kidney
transplant recipients: incidence and association with clinical
and demographic factors. Acta Med Port. 2013;
: 123-6.
Pinho A, Gouveia M, Cardoso JC, Xavier MM, Vieira
R, Alves R. Non-melanoma skin cancer in Portuguese
kidney transplant recipients - incidence and risk factors.
An Bras Dermatol. 2016; 91: 455-62. doi: 10.1590/
abd1806-4841.20164891.
Fernandes S, Carrelha A, Marques Pinto G, Nolasco F,
Barroso E, Cardoso J. Skin disease in liver and kidney
transplant recipients referred to the department of dermatology
and venereology. Acta Med Port. 2013; 26:
-63.
Borges-Costa J, Travassos AR, Vasconcelos P, Guerra J,
Santana A, Weigert A, et al. Conhecimento sobre cancro
de pele e hábitos de fotoproteção em transplantados:
estudo descritivo de 127 doentes com transplante renal.
Rev Soc Port Dermatol Venereol. 2012; 70: 313-17.
European Skin Care in Organ Transplant Recipients.
[Acedido em maio de 2018] Disponível em: http://www.
scopenetwork.org/
International Transplant Skin Cancer Collaborative.
[Acedido em maio de 2018] Disponível em: http://www.
itscc.org/
National Institute for Health and Clinical Excellence.
Guidance on cancer services: improving outcomes for
people with skin tumours including melanoma. London:
National Institute for Health and Clinical Excellence;
Zwald FO, Brown M. Skin cancer in solid organ transplant
recipients: advances in therapy and management:
part II. Management of skin cancer in solid organ transplant
recipients. J Am Acad Dermatol. 2011; 65: 263-
doi: 10.1016/j.jaad.2010.11.063.
Hofbauer GF, Anliker M, Arnold A, Binet I, Hunger R,
Kempf W, et al. Swiss clinical practice guidelines for skin
cancer in organ transplant recipients. Swiss Med Wkly.
; 139: 407-15. doi: smw-12725.
Ismail F, Mitchell L, Casabonne D, Gulati A, Newton
R, Proby CM, et al. Specialist dermatology clinics for
organ transplant recipients significantly improve compliance
with photoprotection and levels of skin cancer
awareness. Br J Dermatol. 2006; 155: 916-25. doi:
1111/j.1365-2133.2006.07454.x
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).