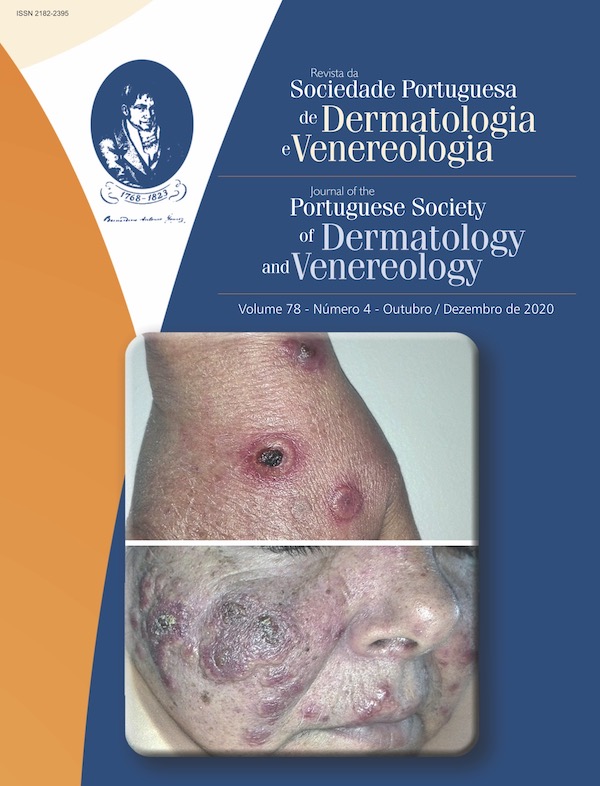
Carcinoma Espinocelular em Doentes com Transplante de Órgão-Sólido
Resumo
Os doentes com transplante de órgão-sólido têm maior incidência de carcinoma espinocelular (CEC) do que a população em geral. Esta maior incidência deve-se a diversos fatores, entre os quais, exposição crónica à radiação ultravioleta, infeção por papiloma vírus humano, fármacos imunossupressores, entre outros. A prevenção primária é crucial, porque além dos CEC serem mais frequentes nos doentes transplantados, são também mais agressivos e têm, portanto, um prognóstico pior. Os novos fármacos imunossupressores estão associados com um risco menor de desenvolvimento de CEC, no entanto, podem ter mais efeitos adversos, levando ao abandono da terapêutica. Em relação às opções terapêuticas para CEC, estas variam entre cirurgia, radioterapia e terapêutica sistémica, apesar de existirem poucos estudos em doentes com transplante de órgão-sólidos, em relação à imunoterapia e inibidores do recetor do fator de crescimento epidérmico.
Downloads
Referências
Rogers W, Weinstock MA, Feldman SR, Coldiron, BM. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015; 151:1081-6. doi: 10.1001/jamadermatol. 2015.1187.
Muzic JG, Schmitt R, Wright AC, Alniemi DT, Zubair AS, Baum CL, et al. Incidence and Trends of Basal Cell Carcinoma and Cutaneous Squamous Cell Carcinoma: A Population-Based Study in Olmsted County, Minnesota, 2000 to 2010. Mayo Clin. Proc. 2017; 92: 890-8. doi: 10.1016/j.mayocp.2017.02.015.
Corchado-Cobos R, García-Sancha N, González-Sarmiento R, Pérez-Losada J, Cañueto J. Cutaneous Squamous Cell Carcinoma: From Biology to Therapy. Int J Mol Sci. 2020; 21:2956. doi: 10.3390/ijms21082956.
Brougham ND, Tan ST. The incidence and risk factors of metastasis for cutaneous squamous cell carcinoma — Implications on the T-classification system. J Surg Oncol. 2014; 110: 876-82. doi: 10.1002/jso.23731.
Leiter U, Keim U, Eigentler T, Katalinic A, Martus P, Garbe C. Incidence, Mortality, and Trends of Nonmelanoma Skin Cancer in Germany. J Investig Dermatol. 2017; 137:1860-7. doi: 10.1016/j.jid.2017.04.020.
Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: Incidence. J Am Acad Dermatol. 1994; 30:774-8.
Bangash HK, Colegio OR. Management of non-melanoma skin cancer in immunocompromised solid organ transplant recipients. Curr Treat Options Oncol. 2012; 13:354–76. doi: 10.1007/s11864-012-0195-3.
Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. N Engl J Med. 2003; 348:1681-91.
Zwald FO, Brown M. Skin cancer in solid organ transplant recipients: advances in therapy and management: part I. Epidemiology of skin cancer in solid organ transplant recipients. J Am Acad Dermatol. 2011; 65:253-61. doi: 10.1016/j.jaad.2010.11.062.
Krynitz B, Olsson H, Lundh B, Lindelof B, Edgren G, Smed KE. Risk of basal cell carcinoma in Swedish organ transplant recipients — a population -based study. Br J Dermatol. 2015; 174:95-103. doi: 10.1111/bjd.14153.
Varra V, Woody NM, Reddy C, Joshi NP, Geiger J, Lamarre, E.D, et al. Suboptimal Outcomes in Cutaneous Squamous Cell Cancer of the Head and Neck with Nodal Metastases. Anticancer Res. 2018; 38: 5825-30. doi: 10.21873/anticanres.12923.
Schmults CD, Karia PS, Carter JB, Han J, Qureshi A. Factors predictive of recurrence and death from cutaneous squamous cell carcinoma: A 10-year, single-institution cohort study. JAMA Dermatol. 2013; 149: 541-7. doi: 10.1001/jamadermatol.2013.2139.
Kim C, Cheng J, Colegio OR. Cutaneous squamous cell carcinomas in solid organ transplant recipients: emerging strategies for surveillance, staging, and treatment. Semin Oncol. 2016; 43:390-4.
Lott DG, Manz R, Koch C, Lorenz R. Aggressive behavior of non-melanotic skin cancers in solid organ transplant recipients. Transplantation. 2010; 90:683-7.
Fernandes S, Carrelha AS, Marques Pinto G, Nolasco F, Barroso E, Cardoso J. Patologia dermatológica em doentes transplantados hepáticos e renais referenciados à consulta de dermatologia e venereologia. Acta Med Port. 2013;26:555-63.
Borges-Costa J, Vasconcelos JP, Travassos AR, Guerra J, Santana A, Weigert A, et al. Cancro Cutâneo em Doentes com Transplante Renal: Incidência e Associações com Fatores Clínicos e Sociodemográficos. Acta Med Port. 2013;26:123-6.
Pinho A, Gouveia M, Cardoso JC, Xavier MM, Vieira R, Alves R. Non-melanoma skin cancer in portuguese kidney transplant recipients – incidence and risk factors. An Bras Dermatol. 2016; 91:455-62.
Garrido PMC, Borges-Costa J. Skin disorders in renal transplant recipients: a retrospective study. An Bras Dermatol. 2017; 92:638-41.
Marcén R, Pascual J, Tato AM, Teruel JL, Villafruela M, Fernández M. et al. Influence of Immunosupression on the prevalence of cancer after kidney transplantation. Transplant Proc. 2003; 35:1714-16.
Fuente MJ, Sabat M, Roca J, Lauzurica R, Fernandéz-Figueras MT, Ferrándiz C. A prospective study of the incidence of skin cancer and its risk factors in a spanish mediterranean population of kidney transplant recipientes. Br J Dermatol. 2003; 149:1221-6.
Naldi L, Fortina AB, Lovati S. Risk of nonmelanoma skin cancer in Italian organ transplant recipients. A registry-based study. Transplantation. 2000; 70:1479-84.
Bibee K, Swartz A, Sridharan S, Kurten CHL, Wessel CB, Skinner H, et al. Cutaneous squamous cell carcinoma in the organ transplant recipient. Oral Oncol. 2020; 103:104562. doi: 10.1016/j.oraloncology.2019.104562.
Plasmeijer EI, Sachse MM, Gebhardt C, Geusau A, Bouwes JN. Cutaneous squamous cell carcinoma (cSCC) and immunosurveillance - the impact of immunosuppression on frequency of cSCC. J Eur Acad Dermatol Venereol. 2019; 33 Suppl 8:33-7. doi: 10.1111/jdv.16025.
Harwood CA, Toland AE, Proby CM, Euvrard S, Hofbauer GFL, Tommasino M, et al. The pathogenesis of cutaneous squamous cell carcinoma in organ transplant recipients. Br J Dermatol. 2017; 177:1217-24. doi: 10.1111/bjd.15956.
Plasmeijer EI, Pandeya N, O'Rourke P, Pawlita M, Waterboer T, Feltkamp MC, et al. The Association between cutaneous squamous cell carcinoma and betapapillomavirus seropositivity: A cohort study. Cancer Epidemiol Biomarkers Prev. 2011; 20:1171-7.
Andersson K, Michael KM, Luostarinen T, Waterboer T, Gislefoss R, Hakulinen T, et al. Prospective study of human papillomavirus seropositivity and risk of nonmelanoma skin cancer. Am J Epidemiol. 2012; 175:685-95.
Quint KD, Genders RE, de Koning MN, Borgogna C, Gariglio M, Bouwes Bavinck JN, et al. Human beta-papillomavirus infection and keratinocyte carcinomas. J Pathol. 2015; 235:342-54.
Howley PM, Pfister HJ. Beta genus papillomaviruses and skin cancer. Virology. 2015; 479-480:290-6.
Chockalingam R, Downing C, Tyring SK. Cutaneous Squamous Cell Carcinomas in Organ Transplant Recipients. J Clin Med. 2015; 4:1229-239.
Weissenborn SJ, Nindl I, Purdie K, Harwood C, Proby C, Breuer J, et al. Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers. J Invest Dermatol. 2005; 125:93-7.
Connolly K, Manders P, Earls P, Epstein RJ. Papillomavirus-associated squamous skin cancers following transplant immunosuppression: One Notch closer to control. Cancer Treat Rev. 2014; 40: 205-14. doi: 10.1016/j.ctrv.2013.08.005.
Burke MT, Isbel N, Barraclough KA, Jung JW, Wells JW, Staatz CE. Genetics and nonmelanoma skin cancer in kidney transplant recipients. Pharmacogenomics. 2015; 16:161-72.
Euvrard S, Morelon E, Rostaing L, Goffin E, Brocard A, Tromme I, et al. Sirolimus and secondary skin-cancer prevention in kidney transplantation. N Engl J Med. 2012; 367:329-39. doi: 10.1056/NEJMoa1204166
Knoll GA, Kokolo MB, Mallick R, Beck A, Buenaventura CD, Ducharme R, et al. Effect of sirolimus on malignancy and survival after kidney transplantation: systematic review and meta-analysis of individual patient data. BMJ. 2014; 349:g6679. doi: 10.1136/bmj.g6679.
Blomberg M, He SY, Harwood C, Arron ST, Demehri S, Green A, et al. Research gaps in the management and prevention of cutaneous squamous cell carcinoma in organ transplant recipients. Br J Dermatol. 2017; 177:1225-33. doi: 10.1111/bjd.15950.
Lloyd A, Klintmalm G, Qin H, Menter A. Skin cancer evaluation in transplant patients: A physician opinion survey with recommendations. Clin Transplant. 2015; 29: 110-7.
Thompson AK, Kelley BF, Prokop LJ, Murad MH, Baum CL. Risk factors for cutaneous squamous cell carcinoma recurrence, metastasis, and disease-specific death: A systematic review and meta-analysis. JAMA Dermatol. 2016; 152:419-28. doi: 10.1001/jamadermatol.2015.4994.
Tam S, Gross ND. Cutaneous Squamous Cell Carcinoma in Immunosuppressed Patients. Curr Oncol Rep. 2019; 21:82. doi: 10.1007/s11912-019-0831-1.
Ulrich C, Bichel J, Euvrard S, Guidi B, Proby CM, van de Kerkhof PCM, et al. Topical immunomodulation under systemic immunosuppression: results of a multicentre, randomized, placebo controlled safety and efficacy study of imiquimod 5% cream for the treatment of actinic keratoses in kidney, heart, and liver transplant patients. Br J Dermatol. 2007;157:25-31.
Ulrich C, Johannsen A, Rowert-Huber J, Ulrich M, Sterry W, Stockfleth E. Results of a randomized, placebo-controlled safety and efficacy study of topical diclofenac 3% gel in organ transplant patients with multiple actinic keratoses. Eur J Dermatol. 2010; 20:482-8.
Ulrich C, Busch JO, Meyer T, Nindl I, Schmook T, Sterry W, et al. Successful treatment of multiple actinic keratoses in organ transplant patients with topical 5% imiquimod: a report of six cases. Br J Dermatol. 2006; 155:451e454.
Ulrich C, Bichel J, Euvrard S, Guidi B, Proby CM, van de Kerkhof PC, et al. Topical immunomodulation under systemic immunosuppression: results of a multicentre, randomized, placebo-controlled safety and efficacy study of imiquimod 5% cream for the treatment of actinic keratoses in kidney, heart, and liver transplant patients. Br J Dermatol. 2007; 157:25e31.
Togsverd-Bo K, Halldin C, Sandberg C, Gonzalez H, Wennberg AM, Sørensen SS, et al. Photodynamic therapy is more effective than imiquimod for actinic keratosis in organ transplant recipients: a randomized intraindividual controlled trial. Br J Dermatol. 2018; 178:903-9. doi: 10.1111/bjd.15884.
Alam M, Ratner D. Cutaneous squamous-cell carcinoma. N Engl J Med. 2001; 344:975-83.
Brodland DG, Zitelli JA. Surgical margins for excision of primary cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1992; 27:241-8.
Kim JYS, Kozlow JH, Mittal B, et al. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2018; 78:560-78.
Locke J, Karimpour S, Young G, Lockett MA, Perez CA. Radiotherapy for epithelial skin cancer. Int J Radiat Oncol Biol Phys. 2001; 51:748-55.
McCord MW, Mendenhall WM, Parsons JT, Flowers FP. Skin cancer of the head and neck with incidental microscopic perineural invasion. Int J Radiat Oncol Biol Phys. 1999; 43:591-5.
Waxweiler W, Sigmon JR, Sheehan DJ. Adjunctive radiotherapy in the treatment of cutaneous squamous cell carcinoma with perineural invasion. J Surg Oncol. 2011; 104:104-5.
Gellrich FF, Hüning S, Beissert S, Eigentler T, Stockfleth E, Gutzmer R, Meier F. Medical treatment of advanced cutaneous squamous-cell carcinoma. J Eur Acad Dermatol Venereol. 2019;33 Suppl 8:38-43.
Maubec E, Petrow P, Duvillard P, Laouenan C, Duval X, Lacroix L, et al. Cetuximab as first-line monotherapy in patients with skin unresectable squamous cell carcinoma: final results of a phase II multicenter study. J Clin Oncol 2010; 29:3419-26.
Foote MC, McGrath M, Guminski A, Hughes BGM, Meakin J, Thomson D, et al. Phase II study of single-agent panitumumab in patients with incurable cutaneous squamous cell carcinoma. Ann Oncol. 2014; 25:2047-52.
Migden MR, Rischin D, Schmults CD, Guminski A, Hauschild A, Lewis KD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018; 379:341-51.
Herold M, Good AJ, Nielson CB, Longo MI. Use of Topical and Systemic Retinoids in Solid Organ Transplant Recipients: Update and Review of the Current Literature. Dermatol Surg. 2019; 45:1442-9.
De Sévaux RG, Smit JV, de Jong EM, van de Kerkhof PC, et al. Acitretin treatment of premalignant and malignant skin disorders in renal transplant recipients: clinical effects of a randomized trial comparing two doses of acitretin. J Am Acad Dermatol. 2003; 49:407-12.
Otley CC, Stasko T, Tope WD, Lebwohl M. Chemoprevention of nonmelanoma skin cancer with systemic retinoids: practical dosing and management of adverse effects. Dermatol Surg. 2006; 32:562-8.
Zwald FO, Brown M. Skin cancer in solid organ transplant recipients: Advances in therapy and management. Part II: Management of skin cancer in solid organ transplant recipients. J Am Acad Dermatol. 2011; 65: 263-79. doi: 10.1016/j.jaad.2010.11.063.
Jirakulaporn T, Endrizzi B, Lindgren B, Mathew J, Lee PK, Dudek AZ. Capecitabine for skin cancer prevention in solid organ transplant recipients. Clin Transplant 2011; 25:541-8. doi: 10.1111/j.1399-0012.2010.01348.x.
Direitos de Autor (c) 2020 Revista da Sociedade Portuguesa de Dermatologia e Venereologia

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Todos os artigos desta revista são de acesso aberto sob a licença internacional Creative Commons Attribution-NonCommercial 4.0 (CC BY-NC 4.0).