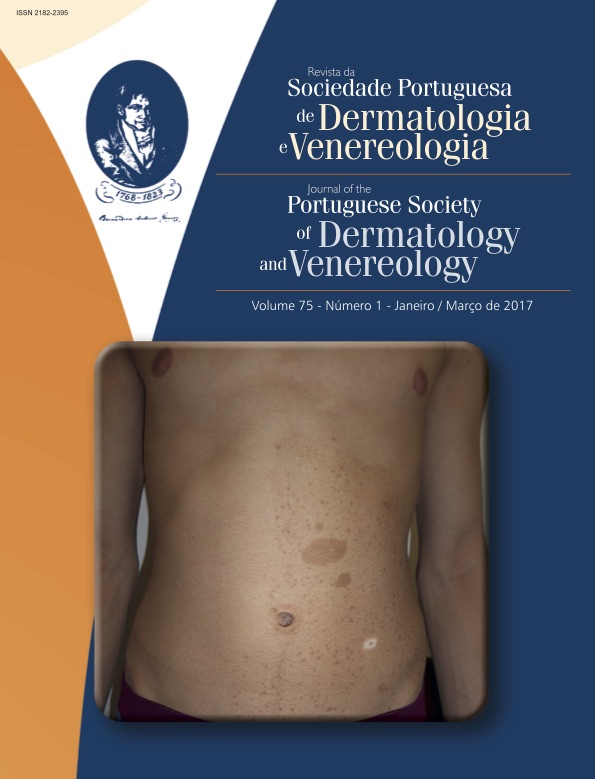
Manifestações Cutâneas das Rasopatias
Resumo
As rasopatias são doenças do desenvolvimento associadas a mutações da via RAS/MAPK. Nos últimos anos, o estudo das vias de sinalização intracelular permitiu a caraterização deste grupo de doenças genéticas, com manifestações clínicas variáveis e dependentes do gene afetado. As rasopatias podem associar-se a alterações do desenvolvimento cognitivo, doenças cardiovasculares, dismorfismo facial e manifestações cutâneas, assim como a um risco aumentado de neoplasias. Entre estas doenças incluem-se a síndrome de Noonan, a síndrome de LEOPARD, a neurofibromatose tipo 1, a síndrome de Legius, a síndrome de Costello e a síndrome cardio-facio-cutânea. O conhecimento das suas manifestações cutâneas é importante, uma vez que pode ajudar a estabelecer o diagnóstico clínico.
Downloads
Referências
Ashton-Beaucage D, Therrien M. How Genetics Has Helped
Piece Together the MAPK Signaling Pathway. Methods
Mol Biol. 2017;1487: 1-21.
Tidyman WE, Rauen KA. The RASopathies: developmental
syndromes of Ras/MAPK pathway dysregulation. Curr
Opin Genet Dev. 2009; 19:230-6.
Niemeyer CM. RAS diseases in children. Haematologica.
;99:1653-62.
Der CJ, Krontiris TG, Cooper GM. Transforming genes
of human bladder and lung carcinoma cell lines are
homologous to the ras genes of Harvey and Kirsten sarcoma
viruses. Proc Natl Acad Sci USA. 1982; 79: 3637-40.
Ishioka C, Ballester R, Engelstein M, Vidal M, Kassel J, The
I, et al. A functional assay for heterozygous mutations in
the GTPase activating protein related domain of the neurofibromatosis type 1 gene. Oncogene. 1995 2; 10: 841-7.
Bos JL. Ras Oncogenes in Human Cancer: a Review.
Cancer Res. 1989; 49: 4682-9.
Hernández-Martín, Torrelo A. Rasopatías: trastornos del
desarrollo con predisposición al cáncer y manifestaciones
cutaneas. Actas Dermosifiliogr. 2011; 102:402-16.
Nava C, Hanna N, Michot C, Pereira S, Pouvreau N,
Niihori T, et al. Cardio-facio-cutaneous and Noonan
syndromes due to mutations in the RAS/MAPK signalling
pathway: genotype-phenotype relationships and overlap
with Costello syndrome. J Med Genet. 2007; 44:763-71.
Smpokou P, Zand DJ, Rosenbaum KN, Summar ML. Malignancy
in Noonan syndrome and related disorders. Clin
Genet 2015: 88:516-22.
Heredia Ramírez CE, Barros F, Barreiro Conde J, Castro-
-Feijóo L, Cabanas Rodríguez P, Pombo Arias M. Rasopatías.
Rev Esp Endocrinol Pediatr 2013; 4:68-86.
Hasle H. Malignant diseases in Noonan syndrome and
related disorders. Horm Res. 2009; 72(Suppl 2):8-14.
Loh ML, Vattikuti S, Schubbert S, et al. Mutations in
PTPN11 implicates the SHP-2 phosphatase in leukemogenesis.
Blood. 2004; 103:2325-31.
Nemes E, Farkas K, Kocsis-Deák B, Drubi A, Sulák A, Tripolszki K, Dósa P, Ferenc L, Nagy N, Széll M. Phenotypical
diversity of patients with LEOPARD syndrome carrying the
worldwide recurrent p.Tyr279Cys PTPN11 mutation. Arch
Dermatol Res. 2015; 307:891-5.
Limongelli G, Pacileo G, Marino B, Digilio MC, Sarkozy A,
Elliott P, et al. Prevalence and clinical significance of cardiovascular abnormalities in patients with the LEOPARD
syndrome. Am J Cardiol. 2007; 100:736-41.
Carcavilla A, Santomé JL, Pinto I, Sánchez-Pozo J, Guillén-
Navarro E, Martín-Frías M, et al. LEOPARD syndrome:
a variant of Noonan syndrome strongly associated with
hypertrophic cardiomyopathy. Rev Esp Cardiol. 2013;
:350-6.
Sarkozy A, Conti E, Digilio MC, Marino B, Morini E, Pacileo
G, et al. Clinical and molecular analysis of 30 patients
with multiple lentigines LEOPARD syndrome. J Med
Genet. 2004; 41:e68.
Zhang Z, Cheng R, Liang J, Ni C, Li M, Yao Z. Lentiginous
phenotypes caused by diverse pathogenic genes (SASH1
and PTPN11): clinical and molecular discrimination. Clin
Genet. 2016; 90:372-7.
Hernández-Martín A, Duat-Rodríguez A. An update on
neurofibromatosis type 1: not just café-au-lait spots, freckling,
and neurofibromas. An update. Part I. dermatological
clinical criteria diagnostic of the disease. Actas
Dermosifiliogr. 2016; 107:454-64.
Viskochil D, Buchberg AM, Xu G, Cawthon RM, Stevens J,
Wolff RK, et al. Deletions and a translocation interrupt a
cloned gene at the neurofibromatosis type 1 locus. Cell.
:62:187.
Ratner N, Miller SJ. A RASopathy gene commonly mutated
in cancer: the neurofibromatosis type 1 tumor suppressor.
Nat Rev Cancer. 2015; 15:290-301.
Neurofibromatosis. Conference statement. National Institutes
of Health Consensus Development Conference.
Arch Neurol. 1988; 45:575-8.
DeBella K, Szudek J, Friedman JM. Use of the National
Institutes of Health criteria for diagnosis of neurofibromatosis
in children. Pediatrics 2000; 105:608-14.
Brems H, Chmara M, Sahbatou M, Denayer E, Taniguchi
K, Kato R, et al. Germline loss-of-function mutations in
SPRED1 cause a neurofibromatosis 1-like phenotype. Nat
Genet. 2007; 39:1120-6.
Serra E, Rosenbaum T, Winner U, Aledo R, Ars E, Estivill
X, et al. Schwann cells harbor the somatic NF1 mutation
in neurofibromas: Evidence of two different Schwann cell
subpopulations. Hum Mol Genet. 2000; 9:3055-64.
Hernández-Martín A, Duat-Rodríguez A. An update on
neurofibromatosis type 1: not just café-au-lait spots and
freckling. Part ii. Other skin manifestations characteristic
of nf1. nf1 and cancer. Actas Dermosifiliogr. 2016;
:465-73.
Hernandez-Martin A, Garcia-Martinez FJ, Duat A, Lopez-
-Martin I, Noguera-Morel L, Torrelo A. Nevus anemicus:
A distinctive cutaneous finding in neurofibromatosis type
Pediatr Dermatol. 2015; 32:342-7.
Marque M, Roubertie A, Jaussent A, Carneiro M, Meunier
L, Guillot B, Pinson L, Pinson S, Bessis D. Nevus anemicus
in neurofibromatosis type 1: a potential new diagnostic
criterion. J Am Acad Dermatol. 2013; 69:768-75.
Fenot M, Stalder JF, Barbarot S. Juvenile xanthogranulomas
are highly prevalent but transient in young children
with neurofibromatosis type 1. J Am Acad Dermatol.
; 71:389-90.
Brems H, Park C, Maertens O, Pemov A, Messiaen L,
Upadhyaya M, et al. Glomus tumors in neurofibromatosis
type 1: genetic, functional, and clinical evidence of a
novel association. Cancer Res. 2009; 69:7393-401.
Kumar MG, Emnett RJ, Bayliss SJ, Gutmann DH. Glomus
tumors in individuals with neurofibromatosis type 1. J Am
Acad Dermatol. 2014; 71:44-8.
Allouche J, Bellon N, Saidani M, Stanchina-Chatrousse
L, Masson Y, Patwardhan A, et al. In vitro modeling of
hyperpigmentation associated to neurofibromatosis type
using melanocytes derived from human embryonic
stem cells. Proc Natl Acad Sci U S A. 2015; 112: 9034-9.
Hirbe AC, Gutmann DH. Neurofibromatosis type 1: a
multidisciplinary approach to care. Lancet Neurol. 2014;
:834-43.
Seminog OO, Goldacre MJ Risk of benign tumours of
nervous system, and of malignant neoplasms, in people
with neurofibromatosis: population-based record-linkage
study. Br J Cancer. 2013; 108:193-8.
Pemov A, Li H, Patidar R, Hansen NF, Sindiri S, Hartley
SW, et al. The primacy of NF1 loss as the driver of
tumorigenesis in neurofibromatosis type 1-associated
plexiform neurofibromas. Oncogene. 2017(in press).
Kiuru M, Busam KJ The NF1 gene in tumor syndromes
and melanoma. Lab Invest. 2017; 97:146-57.
Brems H, Pasmant E, Van Minkelen R, Wimmer K,
Upadhyaya M, Legius E, et al. Review and update of
SPRED1 mutations causing Legius syndrome. Hum Mutat.
; 33:1538-46.
Pasmant E, Ballerini P, Lapillonne H, Perot C, Vidaud D,
Leverger G, et al. SPRED1 disorder and predisposition to
leukemia in children. Blood 2009: 114:1131
Hirata Y, Brems H, Suzuki M, Kanamori M, Okada M, Morita
R, et al. Interaction between a Domain of the Negative
Regulator of the Ras-ERK Pathway, SPRED1 Protein, and
the GTPase-activating Protein-related Domain of Neurofibromin
Is Implicated in Legius Syndrome and Neurofibromatosis
Type 1. J Biol Chem. 2016; 291:3124-34.
Pasmant E, Gilbert-Dussardier B, Petit A, de Laval B, Luscan
A, Gruber A, et al. SPRED1, a RAS MAPK pathway
inhibitor that causes Legius syndrome, is a tumour suppressor
downregulated in paediatric acute myeloblastic
leukaemia. Oncogene. 2015; 34:631-8.
Gripp KW, Lin AE, Stabley DL, Nicholson L, Scott Jr CI,
Doyle D, et al. HRAS mutation analysis in Costello syndrome:
genotype and phenotype correlation. Am J Med
Genet A. 2006; 140:1-7.
Lin AE, Grossfeld PD, Hamilton RM, Smoot L, Gripp KW,
Proud V, et al. Further delineation of cardiac abnormalities
in Costello syndrome. Am J Med Genet A. 2002;
:115-29.
Siege DH, Man JA, Krol AL, Rauen KA. Dermatological
Phenotype in Costello Syndrome: Consequences of Ras
Dysregulation in Development. Br J Dermatol. 2012;
:601-7.
Rauen KA, Schoyer L, McCormick F, Lin AE, Allanson JE,
Stevenson DA, et al. Proceedings from the 2009 genetic
syndromes of the Ras/MAPK pathway: From bedside to
bench and back. Am J Med Genet A. 2010; 152A:4-24.
Gripp KW. Tumor predisposition in Costello syndrome.
Am J Med Genet C Semin Med Genet. 2005; 137C:72-7.
Beukers W, Hercegovac A, Zwarthoff EC. HRAS mutations
in bladder cancer at an early age and the possible association
with the Costello Syndrome. Eur J Hum Genet.
; 22:837-9.
Niihori T, Aoki Y, Narumi Y, Neri G, Cave H, Verloes A, et
al. Germline KRAS and BRAF mutations in cardio-facio-
-cutaneous syndrome. Nat Genet. 2006; 38:294-6.
Dentici, MLSarkozy A, Pantaleoni F, Carta C, Lepri F, Ferese
R, et al. Spectrum of MEK1 and MEK2 gene mutations
in cardio-facio-cutaneous syndrome and genotype–phenotype
correlations. Eur J Hum Genet. 2009; 17:733-40.
Roberts A, Allanson J, Jadico SK, Kavamura MI, Noonan
J, Opitz JM, et al. The cardiofaciocutaneous syndrome. J
Med Genet. 2006; 43:833-42.
Pierpont ME, Magoulas PL, Adi S, Kavamura MI, Neri G,
Noonan J, et al. Cardio-facio-cutaneous syndrome: clinical
features, diagnosis, and management guidelines.
Pediatrics. 2014; 134: e1149–e1162.
Siegel DH, McKenzie J, Frieden IJ, Rauen KA. Dermatologic
findings in 61 mutation-positive individuals with
cardio-facio- cutaneous syndrome. Br J Dermatol. 2011;
:521-9.
Niihori T, Aoki Y, Narumi Y, Neri G, Cave H, Verloes A, et
al. Germline KRAS and BRAF mutations in cardio-facio-
-cutaneous syndrome. Nat Genet. 2006; 38:294-6.
Al-Rahawan MM, Chute DJ, Sol-Church K, Gripp KW, Stabley
DL, McDaniel NL, et al. Hepatoblastoma and heart
transplan- tation in a patient with cardio-facio-cutaneous
syndrome. Am J Med Genet A. 2007; 143A:1481-8.
Korf B, Ahmadian R, Allanson J, Aoki Y, Bakker A, Wright
EB, et al. The third international meeting on genetic disorders
in the RAS/MAPK pathway: towards a therapeutic
approach. Am J Med Genet A. 2015; 167A:1741-6.
Todos os artigos desta revista são de acesso aberto sob a licença internacional Creative Commons Attribution-NonCommercial 4.0 (CC BY-NC 4.0).