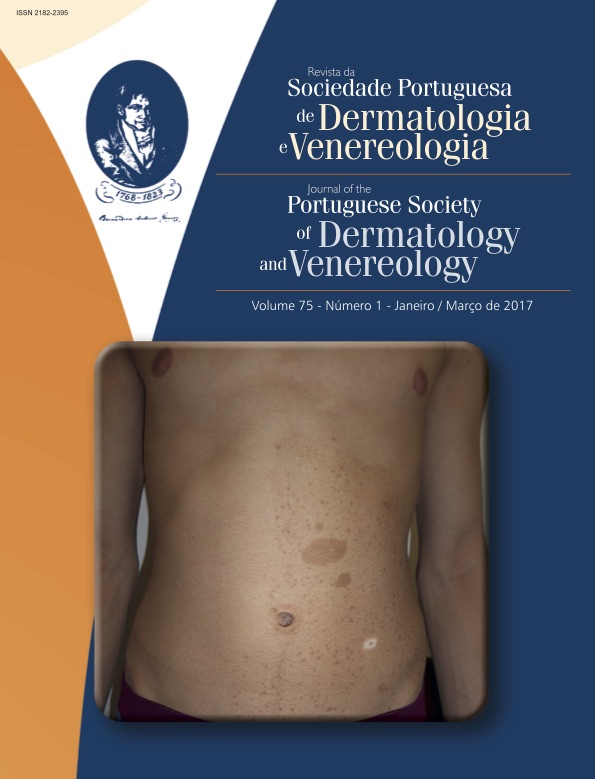
Psoríase, Psicofármacos e Comorbilidades Psiquiátricas: Um Estudo de Caso-Controlo numa População de Doentes Hospitalizados
Resumo
Introdução: A psoríase é uma dermatose inflamatória crónica com impacto significativo na qualidade de vida e múltiplas comorbilidades, com reconhecimento classicamente atribuído aos fatores de risco cardiovascular. Recentemente tem-se destacado a relação com as comorbilidades psiquiátricas.
Material e Métodos: Estabeleceu-se como objetivo primário avaliar a prevalência de psicofármacos na medicação habitual dos doentes hospitalizados com o diagnóstico de psoríase. Realizou-se um estudo de caso-controlo no Serviço de Dermatologia do Centro Hospitalar e Universitário de Coimbra, entre 2010 e 2015, partindo da medicação habitual. Os fármacos foram agrupados pela classificação do INFARMED. Definiram- -se como objetivos secundários comparar a prevalência de fármacos para tratamento de fatores de risco cardiovascular nos dois grupos e reunir informação sobre comorbilidades psiquiátricas disponível nos processos clínicos dos doentes hospitalizados com psoríase. A análise estatística foi realizada recorrendo ao software STATA 14 e a significância estatística foi definida para p<0,05.
Resultados: O grupo com psoríase era constituído por 79 doentes, 67% do sexo masculino, 33% do sexo feminino e idade média de 59,30±17,17 anos. Observou-se uma associação entre psoríase e consumo de fármacos do sistema nervoso central, particularmente psicofármacos, sobretudo ansiolíticos e antipsicóticos (p<0,01), com 63% dos doentes medicados com pelo menos um psicofármaco. Verificou-se também associação entre psoríase e medicação regular com anti-hipertensores (p<0,05). A referência a diagnósticos psiquiátricos nos processos clínicos era, frequentemente, imprecisa ou inexistente.
Conclusão: Os resultados salientam o peso do consumo de psicofármacos e reforçam estudos prévios sobre a subavaliação em psicopatologia dos doentes com psoríase. Salienta-se a importância da avaliação holística nas patologias da psicodermatologia.
Downloads
Referências
Coimbra S, Oliveira H, Figueiredo A, Rocha-Pereira P,
Santos-Silva A. Factors associated with the length of remission
of psoriasis vulgaris. Clin Drug Investig. 2013;
:855-60.
Ferreira BI, Abreu JL, Reis JP, Figueiredo AM. Psoriasis
and associated psychiatric disorders: a systematic review
on etiopathogenesis and clinical correlation. J Clin Aesthet
Dermatol. 2016; 9:36-43.
Hunter HJ, Griffiths CE, Kleyn CE. Does psychosocial
stress play a role in the exacerbation of psoriasis? Br J
Dermatol. 2013; 169:965-74.
Kumar S, Kachhawha D, Das Koolwal G, Gehlot S, Awasthi
A. Psychiatric morbidity in psoriasis patients: a pilot
study. Indian J Dermatol Venereol Leprol. 2011; 77:625.
Heller MM, Lee ES, Koo JY. Stress as an influencing factor
in psoriasis. Skin Therapy Lett. 2011; 16:1-4.
Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB,
Augustin M. Psoriasis: is the impairment to a patient's
life cumulative? J Eur Acad Dermatol Venereol. 2010;
:989-1004.
Rapp SR, Feldman SR, Exum ML, Fleischer AB Jr, Reboussin
DM. Psoriasis causes as much disability as other
major medical diseases. J Am Acad Dermatol. 1999;
:401-7.
American Psychiatric Association. Diagnostic and Statistical
Manual of Mental Disorders.5th ed. Arlington: APA;
Chamoun A, Goudetsidis L, Poot F, Bourdeaud'hui F, Titeca
G. Psoriasis et depression. Rev Med Brux. 2015;
:23-8.
Fleming P, Bai JW, Pratt M, Sibbald C, Lynde C, Gulliver
WP. The prevalence of anxiety in patients with psoriasis:
a systematic review of observational studies and clinical
trials. J Eur Acad Dermatol Venereol. 2016 (in press).
Evers AW, Verhoeven EW, Kraaimaat FW, de Jong EM, de
Brouwer SJ, Schalkwijk J, et al. How stress gets under the
skin: cortisol and stress reactivity in psoriasis. Br J Dermatol.
; 163:986-91.
Mizara A, Papadopoulos L, McBride SR. Core beliefs
and psychological distress in patients with psoriasis
and atopic eczema attending secondary care: the role
of schemas in chronic skin disease. Br J Dermatol. 2012;
:986-93.
Torres-Hernández M, López-García S, Pedroza-Escobar
D, Escamilla-Tilch M. The role of alexithymia as a psychosomatic
factor in psoriasis. Rev Med Inst Mex Seguro Soc.
; 53:268-72.
Naldi L, Parazzini F, Brevi A, Peserico A, Veller Fornasa C,
Grosso G, et al. Family history, smoking habits, alcohol
consumption and risk of psoriasis. Br J Dermatol. 1992;
:212-7.
McAleer MA, Mason DL, Cunningham S, O'Shea SJ, Mc-
Cormick PA, Stone C, et al. Alcohol misuse in patients
with psoriasis: identification and relationship to disease
severity and psychologicaldistress. Br J Dermatol. 2011;
:1256-61.
Kim N, Thrash B, Menter A. Comorbidities in psoriasis
patients. Semin Cutan Med Surg. 2010; 29:10-5.
Bouguéon K, Misery L. Depression and psoriasis. Ann
Dermatol Venereol. 2008; 135 (Suppl 4):S254-8.
Shutty BG, West C, Huang KE, Landis E, Dabade T, Browder
B, et al. Sleep disturbances in psoriasis. Dermatol
Online J. 2013; 19:1.
Sampogna F, Gisondi P, Tabolli S, Abeni D; IDI Multipurpose
Psoriasis Research on Vital Experiences investigators.
Impairment of sexual life in patients with psoriasis.
Dermatology. 2007; 214:144-50.
Cabete J, Torres T, Vilarinho T, Ferreira A, Selores M.
Erectile dysfunction in psoriasis patients. Eur J Dermatol.
; 24:482-6.
Moon HS, Mizara A, McBride SR. Psoriasis and psycho-
-dermatology. Dermatol Ther. 2013; 3:117-30.
Jafferany M, Franca K. Psychodermatology: basics concepts.
Acta Derm Venereol. 2016; 96:35-7.
Todos os artigos desta revista são de acesso aberto sob a licença internacional Creative Commons Attribution-NonCommercial 4.0 (CC BY-NC 4.0).