Vacinação Contra o Vírus do Papiloma Humano em Dermatologia
Resumo
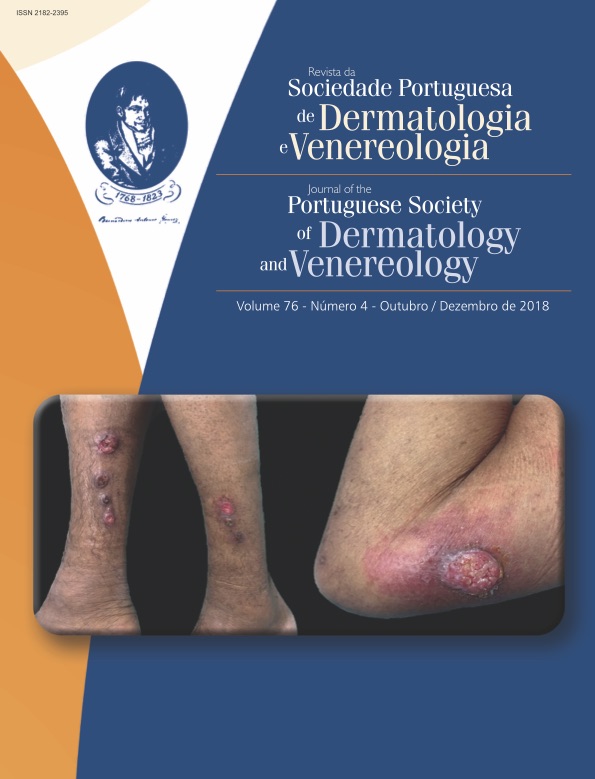
A infeção anogenital pelo vírus do papiloma humano (VPH) é a infeção sexualmente transmissível (IST) mais frequente; devido ao seu potencial oncogénico, está na origem da maioria dos cancros do colo do útero, vulvar, vaginal e anal. Não existe tratamento antiviral específico e o tratamento das neoplasias associadas ao VPH não previne a transmissão. Assim, a prevenção da infeção assume particular relevância e a consulta de Venereologia constitui uma oportunidade privilegiada para aconselhar quem pode beneficiar de medidas preventivas. A mais recente vacina contra o VPH é a nonavalente, proporcionando cobertura para os tipos 6, 11, 16, 18, 31, 33, 45, 52 e 58, que, em conjunto, respondem por 90% dos cancros do colo do útero e condilomas. A vacina é recomendada pela OMS para mulheres e homens até aos 26 anos. Na maioria dos países, a vacina é comparticipada para proporcionar imunização universal gratuita a adolescentes do sexo feminino antes do início da atividade sexual. Para além da população-alvo, a vacina pode beneficiar outros populações-alvo frequentemente tratadas pelos dermatologistas: homens que têm sexo com homens, imunodeprimidos incluindo transplantados e infetados pelo VIH, e candidatos a tratamentos imunossupressores. A decisão de vacinar um indivíduo deve considerar o risco de exposição prévia ao VPH e o benefício potencial da vacinação, que é profilática e não terapêutica. Revemos a evidência publicada sobre a imunogenicidade, segurança e eficácia da vacina contra o VPH em diferentes contextos clínicos e identificamos as recomendações internacionais que podem guiar o aconselhamento individual pelo dermatologista.
Downloads
Referências
De Vuyst H, Clifford G, Li N, Franceschi S. HPV infection in Europe. Eur J Cancer. 2009;45(15):2632–9.
Hariri S, Unger E, Sternberg M, Dunne E, Swan D, Patel S, et al. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J Infect Dis 204566-573. 2011;204(4):566–73.
Gargano J, Unger E, Liu G, Steinau M, Meites E, Dunne E, et al. Prevalence of Genital Human Papillomavirus in Males, United States, 2013-2014. J Infect Dis. 2017;215(7):1070–9.
Pista A, de Oliveira C, Cunha M, Paixão T, Real O. CLEOPATRE Portugal Study Group. Prevalence of Human Papillomavirus Infection in Women in Portugal: The CLEOPATRE Portugal Study. Int J Gynecol Cancer. 2011;21(6):1150–8.
Schiller JT, Lowy DR. Understanding and learning from the success of prophylactic human papillomavirus vaccines. Nat Rev Microbiol. 2012;10(10):681–92.
Li N, Franceschi S, Howell-Jones R, Snijders P, Clifford G. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: variation by geographical region, histological type and year of publication. Int J Cancer. 2011;128(4):927–35.
Direção Geral Da Saúde. Programa Nacional de Vacinação 2017. Ministério da Saúde. 2016.
Moreira EDJ, Block SL, Ferris D, Giuliano AR, Iversen O-E, Joura EA, et al. Safety Profile of the 9-Valent HPV Vaccine: A Combined Analysis of 7 Phase III Clinical Trials. Pediatrics. 2016;138(2):e 20154387.
Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb Mortal Wkly report Recomm reports. 2014;63(5):1–30.
Giuliano A, Palefsky J, Goldstone S, Moreira ED, Penny ME, Aranda C, et al. Efficacy of quadrivalent HPV vaccine against HPV Infection and disease in males. N Engl J Med. 2011;364:401–11.
Read T, Hocking J, Chen M, Donovan B, Bradshaw C, Fairley C. The near disappearance of genital warts in young women 4 years after commencing a national human papillomavirus (HPV) vaccination programme. Sex Transm Infect. 2011;87(7):544–7.
Hestbech MS, Lynge E, Kragstrup J, Siersma V, Baillet MVP, Brodersen J. The impact of HPV vaccination on future cervical screening: A simulation study of two birth cohorts in Denmark. BMJ Open. 2015;5(8):1–7.
Landy R, Windridge P, Gillman MS, Sasieni PD. What cervical screening is appropriate for women who have been vaccinated against high risk HPV? A simulation study. Int J Cancer. 2018;142(4):709–18.
Herrero R, Quint W, Hildesheim A, P G, Struijk L, Katki H, et al. Reduced prevalence of oral human papillomavirus (HPV) 4 years after bivalent HPV vaccination in a randomized clinical trial in Costa Rica. PLoS One. 2013;8:e68329.
Silling S, Wieland U, Werner M, Pfister H, Potthoff A, Kreuter A. Resolution of novel human papillomavirus-induced warts after HPV vaccination. Emerg Infect Dis. 2014;20(1):142–5.
Smith SP, Baxendale HE, Sterling JC. Clearance of recalcitrant warts in a patient with idiopathic immune deficiency following administration of the quadrivalent human papillomavirus vaccine. Clin Exp Dermatol. 2017;42(3):306–8.
Howley P, Lowy D. Papillomaviruses. In: Knipe D, Howley P, editors. Fields virology. 5th ed. Lippincott Williams & Wilkins Philadelphia; 2011. p. 2299–354.
World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017. Wkly Epidemiol Rec. 2017;92(19):241–68.
Stanley M. HPV vaccination in boys and men. Hum Vaccin Immunother. 2014;10(7):2109–11.
Vaz N, Borges-Costa J, Marques MS. Condilomas genitais e associação com cancro. Rev SPDV. 2013;71(1):59–63.
Leite I, Lisboa C, Azevedo F. Vírus do Papiloma Humano e Vacinação. Rev da SPDV. 2011;69(3):395–402.
Hillman R, Giuliano A, Palefsky J, Goldstone S, Moreira E, Vardas E, et al. Immunogenicity of the quadrivalent human papillomavirus (type 6/11/16/18) vaccine in males 16 to 26 years old. Clin Vaccine Immunol. 2012;19(2):261–7.
Palefsky J, Giuliano A, Goldstone S, Moreira E, Aranda C, Jessen H, et al. HPV Vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365(17):1576–85.
Reusser N, Downing C, Guidry J, Tyring S. HPV Carcinomas in Immunocompromised Patients. J Clin Med. 2015;4(2):260–81.
Jamieson DJ, Duerr A, Burk R, Klein RS, Paramsothy P, Schuman P, et al. Group HERS Characterization of genital human papillomavirus infection in women who have or who are at risk of having HIV infection. Am J Obs Gynecol. 2002;186(1):21–27.
Vuyst H De, Lillo F, Broutet N, Smith JS. HIV, human papillomavirus, and cervical neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev. 2008;17:545–554.
Palefsky JM, Holly E, Ralston M, Jay N, Berry J, Darragh T. High incidence of anal high-grade squamous intra-epithelial lesions among HIV-positive and HIV-negative homosexual and bisexual men. AIDS. 1998;12(5):495–503.
Frisch M, Biggar R, Goedert J. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst. 2000;92(18):1500–10.
Kumar D, Unger ER, Panicker G, Medvedev P, Wilson L, Humar A, et al. Immunogenicity of Quadrivalent Human Papillomavirus Vaccine in Organ Transplant Recipients. Am J Transpl. 2013;13(9):2411–7.
Dhar JP, Essenmacher L, Dhar R, Magee A, Ager J, Sokol RJ. The safety and immunogenicity of Quadrivalent HPV (qHPV) vaccine in systemic lupus erythematosus. Vaccine. 2017;35(20):2642–6.
Mok CC, Ho LY, Fong LS, To CH. Immunogenicity and safety of a quadrivalent human papillomavirus vaccine in patients with systemic lupus erythematosus: a case-control study. Ann Rheum Dis. 2013;72(5):659–64.
Wilkin TJ, Chen H, Cespedes MS, Leon-Cruz JT, Godfrey C, Chiao EY, et al. A randomized, placebo-controlled trial of the quadrivalent HPV vaccine in HIV-infected adults age 27 years or older: AIDS Clinical Trials Group protocol A5298 [Internet]. Clin Infect Dis. 2018. p. Apr 5 [cited 2018 Jul 22]. Available from: https://academic.oup.com/cid/article-lookup/doi/10.1093/cid/ciy274 [Epub ahead of print]
Levin MJ, Moscicki A, Song L, Fenton T, Nowak B, Sattler C a, et al. Safety and immunogenicity of a quadrivalent human papillomaviru (types 6, 11, 16, and 18) vaccine in HIV-infected children 7 to 12 years old. J Acquir Immune Defic Syndr. 2010;55(2):197–204.
Lebwohl M, Bagel J, Gelfand J, Gladman D, Gordon K, Hsu S, et al. From the Medical Board of the National Psoriasis Foundation: monitoring and vaccinations in patients treated with biologics for psoriasis. J Am Acad Dermatology. 2008;58(1):94–105.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, et al. 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host. Clin Infect Dis. 2014;58(3):e44–100.
Lopez A, Mariette X, Bachelez H, Belot A, Bonnotte B, Hachulla E, et al. Vaccination recommendations for the adult immunosuppressed patient: A systematic review and comprehensive field synopsis. J Autoimmun. 2017;80:10–27.
Garland SM, Brotherton JML, Moscicki AB, Kaufmann AM, Stanley M, Bhatla N, et al. HPV vaccination of immunocompromised hosts. Papillomavirus Res. 2017;4:35–8.
Emiko Petrosky, Joseph A. Bocchini , Susan Hariri, Harrell Chesson, C. Robinette Curtis, Mona Saraiya, MD5, Elizabeth R. Unger LEM. Use of 9-Valent Human Papillomavirus (HPV) Vaccine: Updated HPV Vaccination Recommendations of the Advisory Committee on Immunization Practices. Mmwr. 2015;64(11):300–4.
Wine-Lee L, Keller SC, Wilck MB, Gluckman SJ, Van Voorhees AS. From the Medical Board of the National Psoriasis Foundation: Vaccination in adult patients on systemic therapy for psoriasis. J Am Acad Dermatol. 2013;69(6):1003–13.
Todos os artigos desta revista são de acesso aberto sob a licença internacional Creative Commons Attribution-NonCommercial 4.0 (CC BY-NC 4.0).