DRUG INDUCED CUTANEOUS REACTIONS – A SERIES OF INPATIENTS DURING AN ELEVEN YEAR PERIOD
Abstract
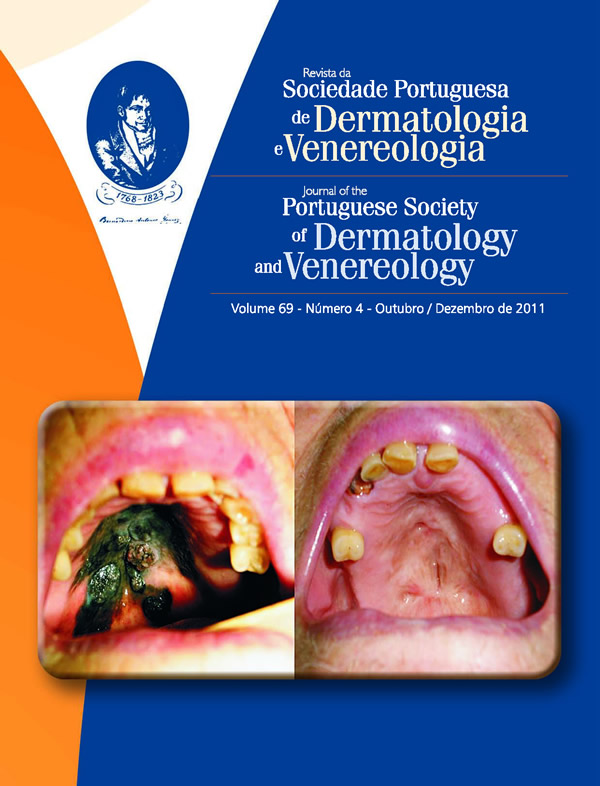
Introduction: The skin and mucosa are common targets of the drug reactions, with a broad range of clinical patterns and drugs involved.
Objective: Our aim was to characterize the drug eruptions requiring hospitalization.
Methods: Clinical and laboratory data of the inpatients with cutaneous drug reactions in our Department during a pe- riod of 11 years (2000-2010) were analyzed.
Results: The study included 168 patients (110 female and 58 male). The clinical patterns were: maculopapular eruption (n=85, 50.6%), Stevens-Johnson Syndrome (SJS: n=14, 8.3%), toxic epidermal necrolysis (TEN: n=10, 5.9 %), SJS/TEN overlap (n=3), drug reaction with eosinophilia and systemic symptoms (DRESS: n=12), photosensivity reaction (n=10 cases), erythroderma (n=9), acute generalized exantematous pustulosis (n=6), fixed drug eruptions (n=6), vasculitis (n=5), erythema multiforme (n=3), urticaria/angioedema (n=2), Sweet syndrome (n=1), symmetrical drug-related intertriginous flexural exanthema (SDRIFE: n=1) and lichenoid eruption (n=1). The drugs most often involved were: antibiotics (39.8%, mostly amoxicillin with clavulanic acid or cotrimoxazole), anticonvulsants (15.5%), nonsteroidal anti-inflammatory drugs (13.1%) and allopurinol (12.5%). Concomitant virus infection was found in 4 patients (Epstein Barr virus, cytomegalovirus, human herpesvirus-6 and parvovirus B19). The median period between drug intake and skin lesion onset was of 8 days (range 6 hours - 90 days). Nineteen patients continued the drug for more than 10 days after the eruption onset; 6 of them developed erythroderma, but none developed SJS/TEN. Most of the patients were treated with systemic corticotherapy and 15 patients received intravenous immunoglobulin. The overall mortality was 5.3%, being 26% for SJS/TEN.
Besides a high SCORTEN, infection and low albumin were related with the mortality in SJS/TEN.
KEYWORDS – Hospitalization; Epidermal Necrolysis, Toxic; Drug Eruptions; Drug Hypersensitivity.
Downloads
All articles in this journal are Open Access under the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0).